卵巢癌作为妇科三大恶性肿瘤之一,死亡率居于首位,5年生存率仅为30%~40%[1]。已知BRCA1/2是遗传性卵巢癌的易感基因, 是参与DNA损伤修复、转录调控、细胞生长控制和遗传完整性保护的抗癌基因,当BRCA1/2基因发生突变时,同源重组发生缺陷,修复双链DNA受损,无法维持遗传稳定性,导致癌症的发生[2-4]。研究表明, BRCA基因未突变者患卵巢癌的风险为1.4%。BRCA1突变者患卵巢癌的风险为44%,BRCA2突变者为17%[5]。
对携带BRCA基因突变者行预防性输卵管卵巢切除术,可降低80%卵巢癌风险;长期使用避孕药预防治疗,携带BRCA1突变者患卵巢癌风险降低了50%,携带BRCA2突变者患卵巢癌风险降低了60%[6-8]。因此,早期发现BRCA基因突变是预防卵巢癌的关键,BRCA基因突变在不同国家和地区存在差异。在本研究中,采用NGS第二代测序方法,对中国东部地区部分卵巢癌患者BRCA基因突变情况进行分析。
对象与方法
一、研究对象
收集2016年1月至2018年12月浙江省肿瘤医院术后病理证实为卵巢癌患者310例,年龄25~80岁,采集术前血清CA125、HE4水平。两名病理学家对样本行BRCA1/2基因检测。该研究得到了伦理委员会的批准,并获得了每位患者的书面知情同意书。
二、BRCA1/2检测
使用BD公司EDTAK2型抗凝真空采血管进行采集,采集外周血送浙江省肿瘤医院病理实验室。AmoyDx核酸提取试剂提取DNA,DNA浓度大于5 ng/μL,总DNA大于450 ng。采用Qubit©dsDNA HS Assay Kit荧光染料法检测DNA浓度。文库浓度≥0.5 ng/μL(2 nM)为质量控制合格;若文库浓度<0.5 ng/μL(2 nM),则质量控制不合格,应重复进行文库质量检查。简单地说,通过PCR扩增构建,适合在Illumina MiSeqDx平台上测序,实现靶区突变检测。PCR扩增反应是在扩增产物的5′端和3′端分别使用具有特定序列(如Tag1和Tag2)的靶区特异性引物对目标序列进行PCR扩增;以第一步的PCR产物为模板,用与Tag1和Tag2序列相同的特异性通用引物进行PCR。用与Tag1和Tag2序列相同的特定通用引物扩增所有目标序列,在目标序列两端添加测序结序列和标记序列,进行PCR。在Illumina MiSeqDx平台上进行测序。测序数据通过“人类12基因高通量测序数据分析软件”中的ADXBRCA模块进行分析,得到BRCA1基因和BRCA2基因的突变结果。
三、统计学分析
采用SPSS 26软件进行统计分析,定量数据正态分布用均数±标准差,偏态分布用中位数(四分位数间距)表示;定性数据用百分率/构成比(%)示。两组间比较采用卡方检验或Mann-Whitney U检验,P值<0.05为差异有统计学意义。
结 果
在310例卵巢癌患者中,浙江省263人占84.8%,其余少部分患者分别来自安徽省22人(7.1%)、江苏省16人(5.2%)和江西省9人(2.9%),见图1。共检测到BRCA基因突变87例(28.1%),其中BRCA1突变64例(20.1%),BRCA2突变23例(8.0%)。在87例BRCA突变中,主要有4种类型的突变,即移码突变(57.5%)、无义突变(26.4%)、错义突变(13.8%)和剪接突变(2.3%),见图2、图3。BRCA1突变中,体系突变11例(17.2%),胚系突变20例(31.3%),两种突变33例(51.5%);在 BRCA2突变中,6个体系突变(26.1%),10个胚系突变(43.5%),7个两种突变都存在(30.4%)。在BRCA1突变患者中共检出45个突变体,其中以c.547-5477del和c.981-982del突变为主。BRCA2突变患者共发现22个突变,其中以c.6373-6374insA突变为主(见表1、表2)。310例卵巢癌患者年龄范围为25~80岁,中位年龄为56岁,平均年龄57岁。BRCA1突变患者的平均年龄略低于BRCA2突变患者的平均年龄,BRCA1/2突变患者的平均年龄与无突变患者的平均年龄相似。BRCA基因与年龄、病理类型、肿瘤标记物CA125、HE4无统计学意义,P均>0.05(见表3)。
表1 BRCA1基因突变体分布
Table 1 Distribution of BRCA1 gene mutants
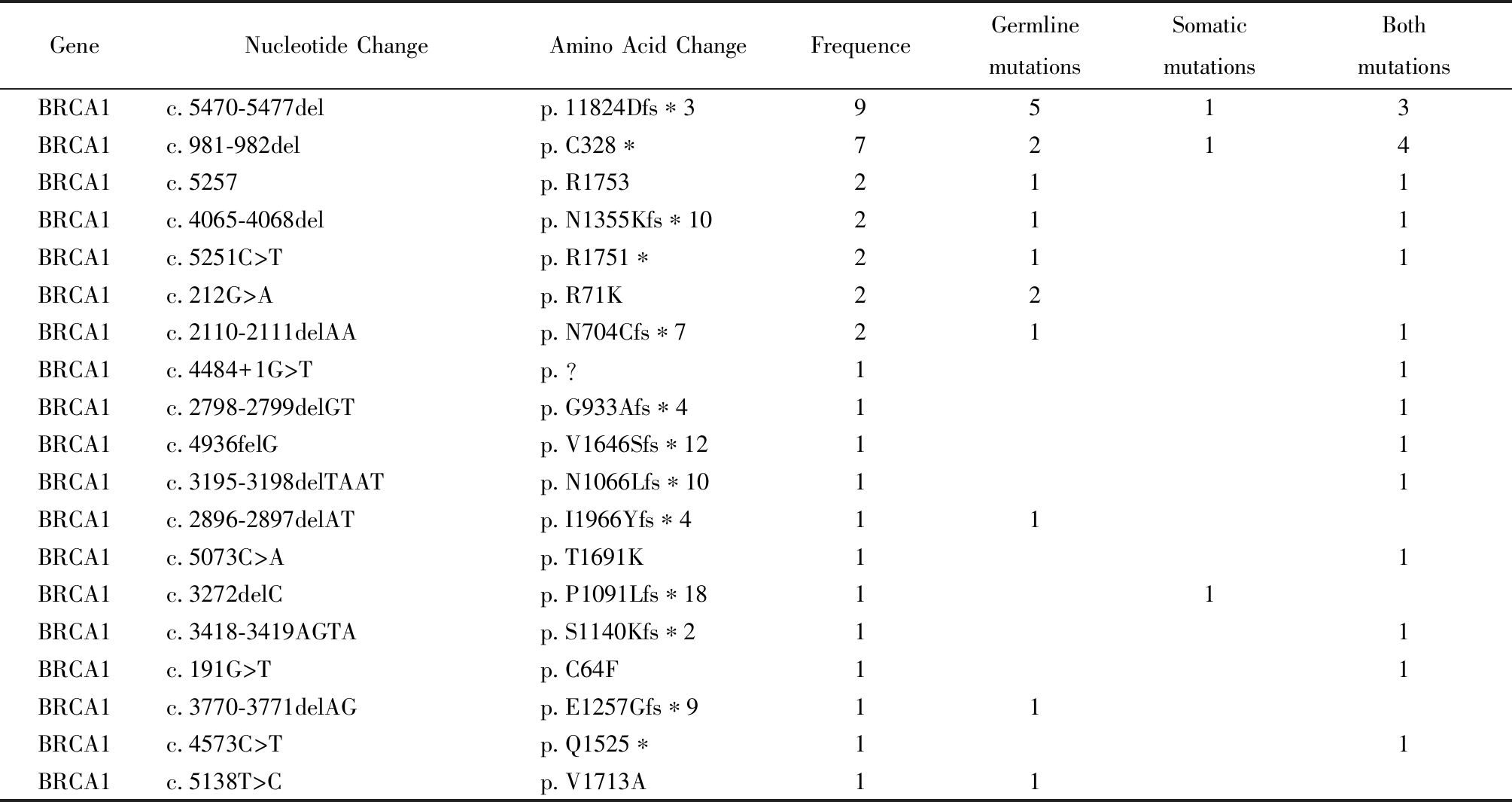
GeneNucleotide ChangeAmino Acid ChangeFrequenceGermline mutationsSomaticmutationsBoth mutationsBRCA1c.5470-5477delp.11824Dfs∗39513BRCA1c.981-982delp.C328∗7214BRCA1c.5257p.R1753211BRCA1c.4065-4068delp.N1355Kfs∗10211BRCA1c.5251C>Tp.R1751∗211BRCA1c.212G>Ap.R71K22BRCA1c.2110-2111delAAp.N704Cfs∗7211BRCA1c.4484+1G>Tp.?11BRCA1c.2798-2799delGTp.G933Afs∗411BRCA1c.4936felGp.V1646Sfs∗1211BRCA1c.3195-3198delTAATp.N1066Lfs∗1011BRCA1c.2896-2897delATp.I1966Yfs∗411BRCA1c.5073C>Ap.T1691K11BRCA1c.3272delCp.P1091Lfs∗1811BRCA1c.3418-3419AGTAp.S1140Kfs∗211BRCA1c.191G>Tp.C64F11BRCA1c.3770-3771delAGp.E1257Gfs∗911BRCA1c.4573C>Tp.Q1525∗11BRCA1c.5138T>Cp.V1713A11
表1(续)
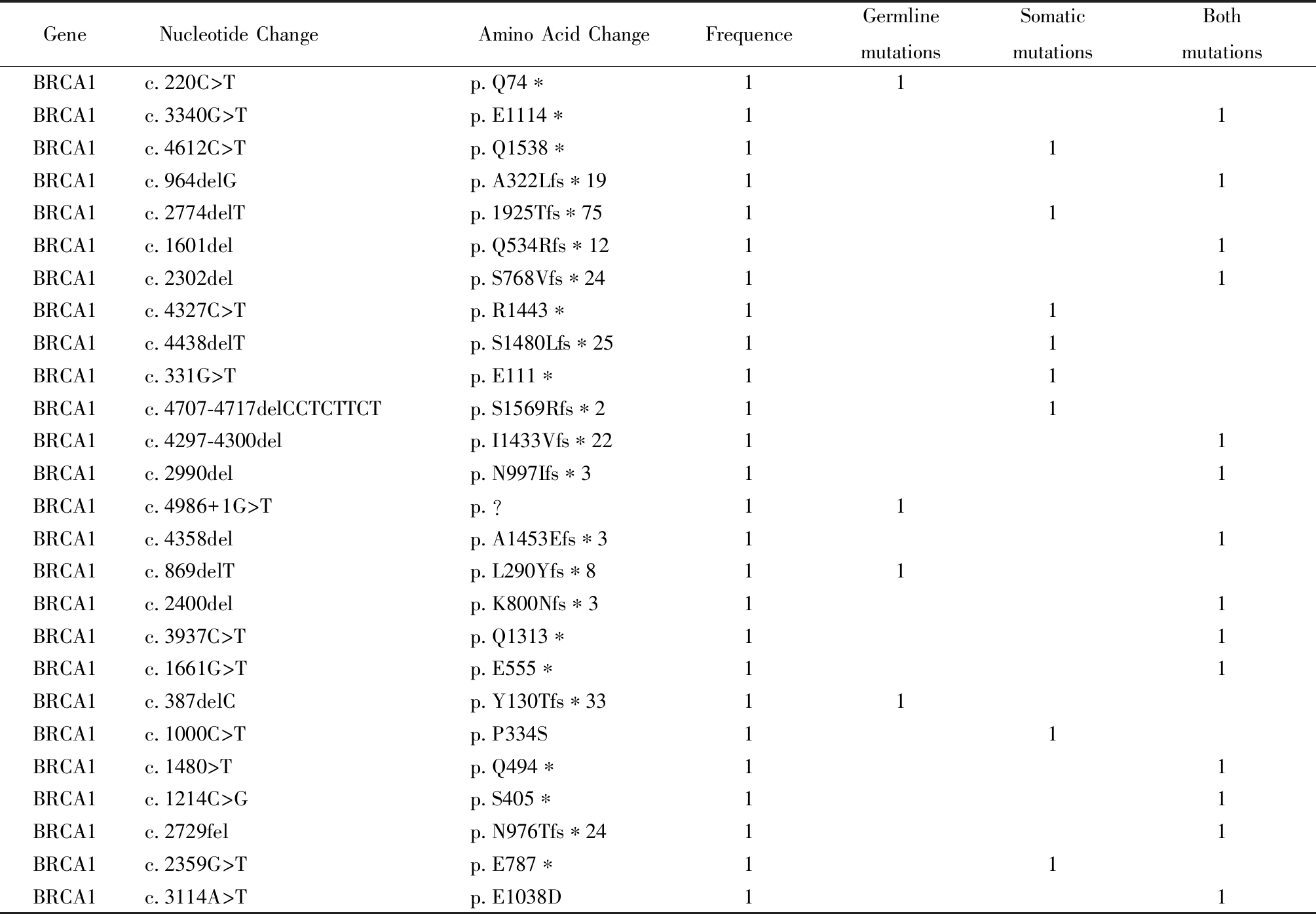
GeneNucleotide Change Amino Acid ChangeFrequenceGermline mutationsSomaticmutationsBoth mutationsBRCA1c.220C>Tp.Q74∗11BRCA1c.3340G>Tp.E1114∗11BRCA1c.4612C>Tp.Q1538∗11BRCA1c.964delGp.A322Lfs∗1911BRCA1c.2774delTp.1925Tfs∗7511BRCA1c.1601delp.Q534Rfs∗1211BRCA1c.2302delp.S768Vfs∗2411BRCA1c.4327C>Tp.R1443∗11BRCA1c.4438delTp.S1480Lfs∗2511BRCA1c.331G>Tp.E111∗11BRCA1c.4707-4717delCCTCTTCTp.S1569Rfs∗211BRCA1c.4297-4300delp.I1433Vfs∗2211BRCA1c.2990delp.N997Ifs∗311BRCA1c.4986+1G>Tp.?11BRCA1c.4358delp.A1453Efs∗311BRCA1c.869delTp.L290Yfs∗811BRCA1c.2400delp.K800Nfs∗311BRCA1c.3937C>Tp.Q1313∗11BRCA1c.1661G>Tp.E555∗11BRCA1c.387delCp.Y130Tfs∗3311BRCA1c.1000C>Tp.P334S11BRCA1c.1480>Tp.Q494∗11BRCA1c.1214C>Gp.S405∗11BRCA1c.2729felp.N976Tfs∗2411BRCA1c.2359G>Tp.E787∗11BRCA1c.3114A>Tp.E1038D11
表2 BRCA2基因突变体分布
Table 2 Distribution of BRCA2 gene mutants
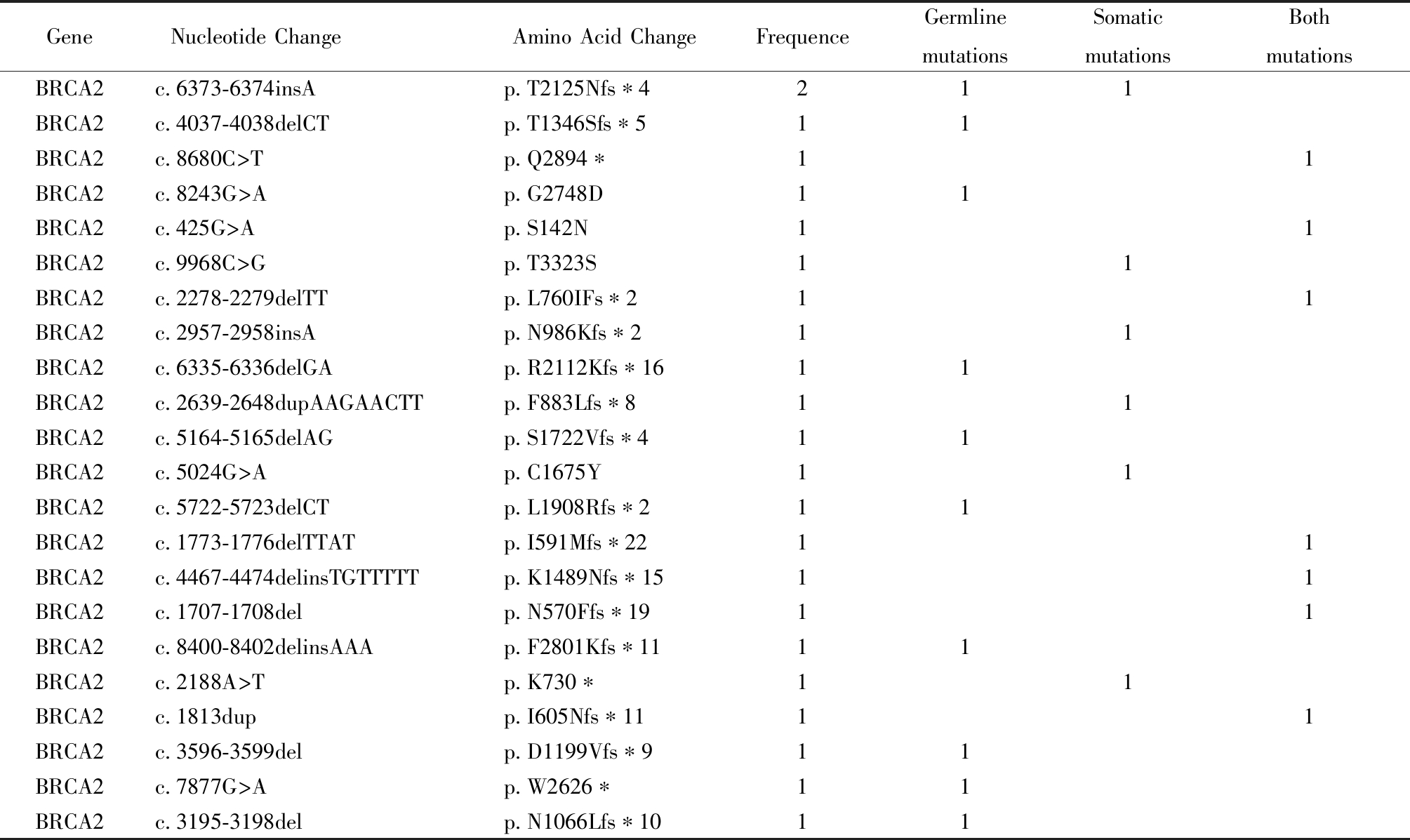
GeneNucleotide Change Amino Acid ChangeFrequenceGermline mutationsSomaticmutationsBoth mutationsBRCA2c.6373-6374insAp.T2125Nfs∗4211BRCA2c.4037-4038delCTp.T1346Sfs∗511BRCA2c.8680C>Tp.Q2894∗11BRCA2c.8243G>Ap.G2748D11BRCA2c.425G>Ap.S142N11BRCA2c.9968C>Gp.T3323S11BRCA2c.2278-2279delTTp.L760IFs∗211BRCA2c.2957-2958insAp.N986Kfs∗211BRCA2c.6335-6336delGAp.R2112Kfs∗1611BRCA2c.2639-2648dupAAGAACTTp.F883Lfs∗811BRCA2c.5164-5165delAGp.S1722Vfs∗411BRCA2c.5024G>Ap.C1675Y11BRCA2c.5722-5723delCTp.L1908Rfs∗211BRCA2c.1773-1776delTTATp.I591Mfs∗2211BRCA2c.4467-4474delinsTGTTTTTp.K1489Nfs∗1511BRCA2c.1707-1708delp.N570Ffs∗1911BRCA2c.8400-8402delinsAAAp.F2801Kfs∗1111BRCA2c.2188A>Tp.K730∗11BRCA2c.1813dupp.I605Nfs∗1111BRCA2c.3596-3599delp.D1199Vfs∗911BRCA2c.7877G>Ap.W2626∗11BRCA2c.3195-3198delp.N1066Lfs∗1011
表3 BRCA基因临床特征描述[例(%)]
Table 3 Description of Clinical Characteristics of BRCA Gen [n(%)]
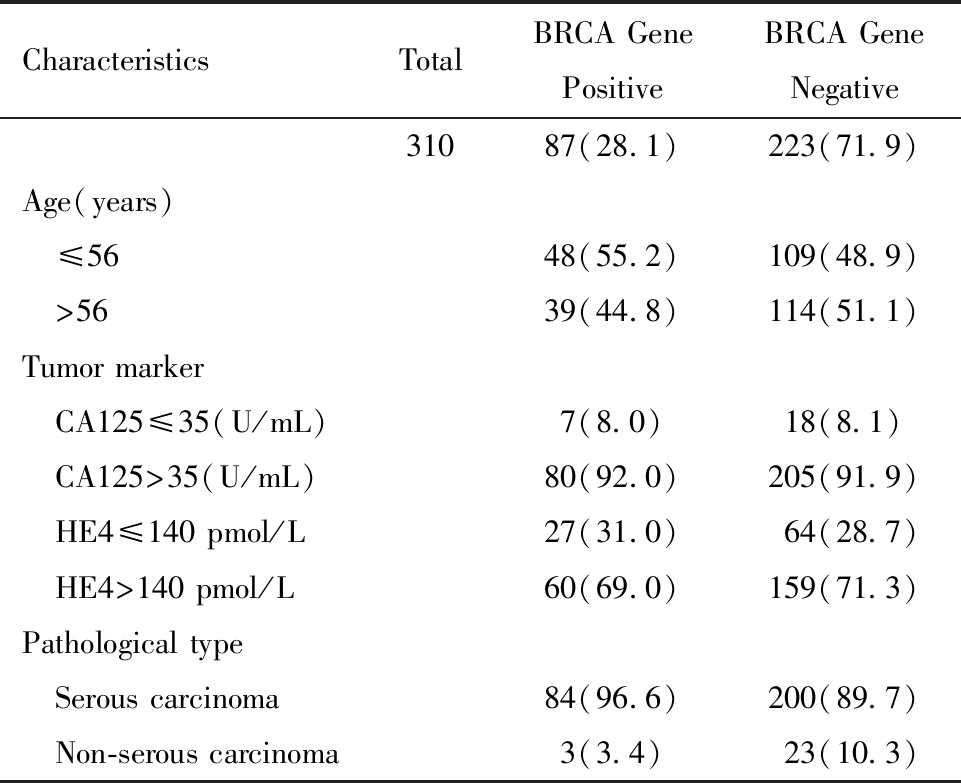
CharacteristicsTotalBRCA GenePositiveBRCA GeneNegative31087(28.1)223(71.9)Age(years) ≤5648(55.2)109(48.9) >5639(44.8)114(51.1)Tumor marker CA125≤35(U/mL)7(8.0)18(8.1) CA125>35(U/mL)80(92.0)205(91.9) HE4≤140 pmol/L27(31.0)64(28.7) HE4>140 pmol/L60(69.0)159(71.3)Pathological type Serous carcinoma84(96.6)200(89.7) Non-serous carcinoma3(3.4)23(10.3)
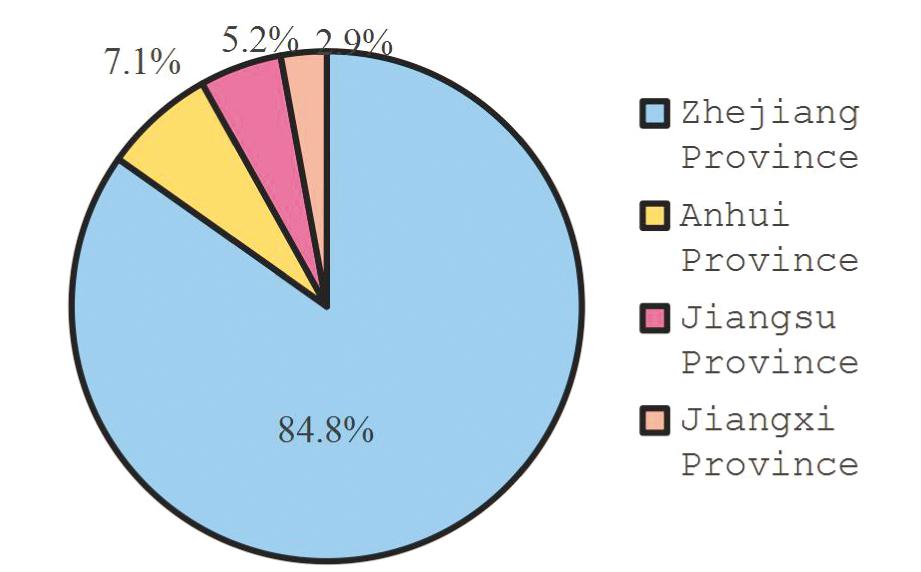
图1 患者省份分布
Figure 1 Province distribution of patients
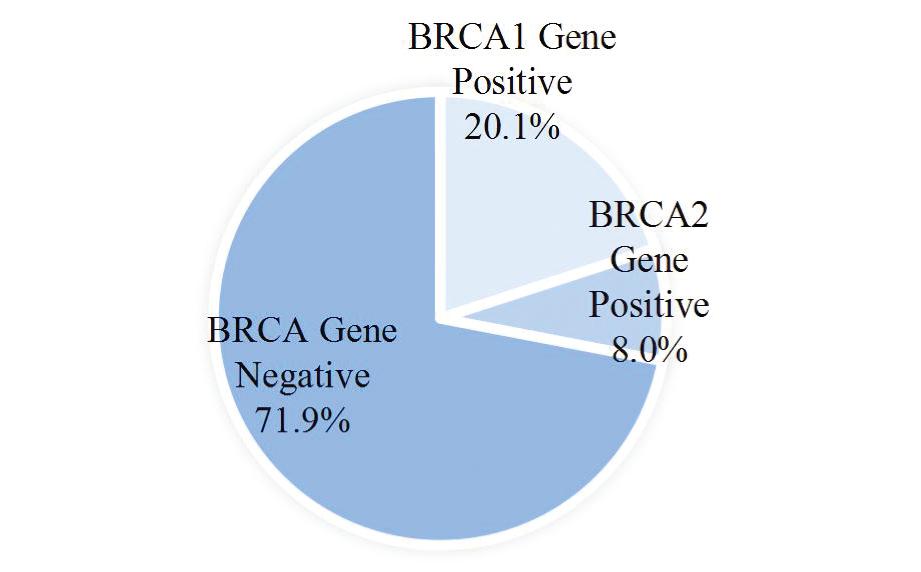
图2 BRCA基因突变率分布
Figure 2 Distribution of BRCA gene mutation rates
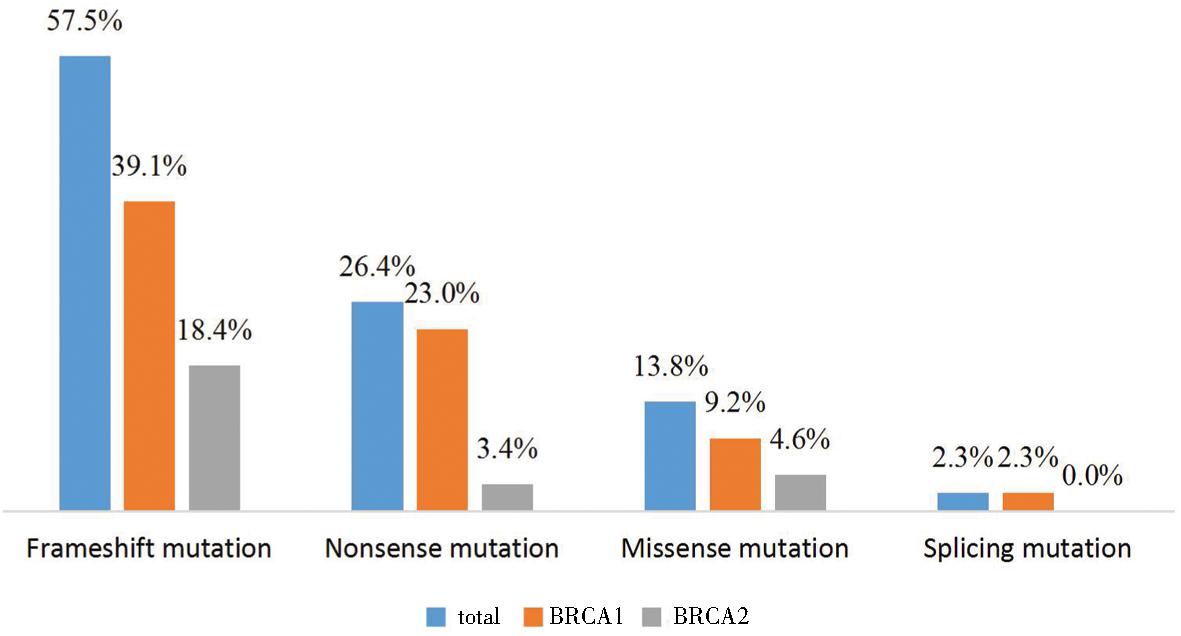
图3 BRCA基因突变类型分布
Figure 3 Distribution of BRCA gene mutations
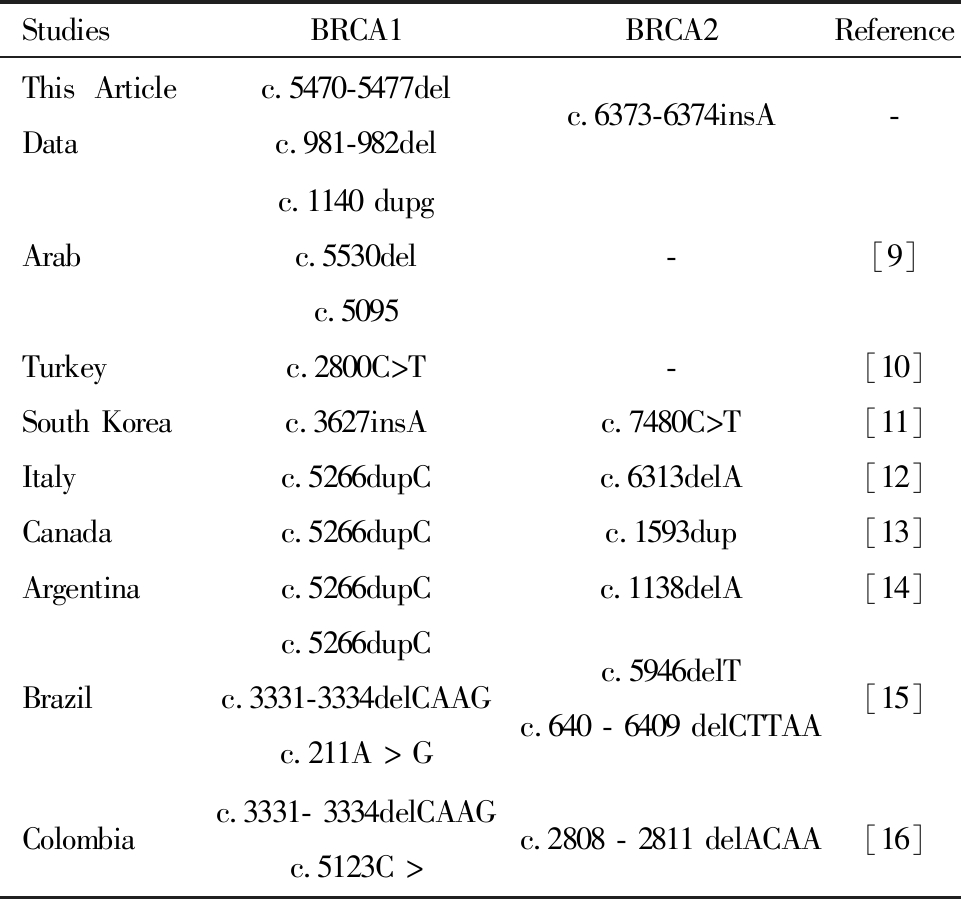
收集不同国家卵巢癌患者BRCA1/2突变体进行比较。本文中最常见BRCA1突变体是c.5470-5477del和c.981-982del, BRCA2突变体最常见突变体是c.6373-6374insA。阿拉伯BRCA1最常见突变体分别为c.1140 dupg、c.5530del、c.5095C>T[9]。土耳其BRCA1最常见突变体c.2800C>T[10]。韩国BRCA1最常见突变体c.3627ins,BRCA2最常见突变体c.7480C>T[11]。意大利BRCA1最常见突变体c.5266dupC, BRCA2最常见突变体c.6313delA[12]。加拿大BRCA1最常见突变体c.5266dupC, BRCA2最常见突变体c.1593dup[13]。阿根廷BRCA1、BRCA2最常见突变体分别为c.5266dupC、c.1138delA[14]。巴西最常见的BRCA1突变体是c.5266dupC、c.3331-3334del、c. 5266dupc、211A>G,最常见BRCA2突变是c.5946delT、c.640-6409delCTTAA[15]。哥伦比亚最常见BRCA1、BRCA2突变体分别为c.3331- 3334delcaag、c. 3334、5123C>A、c.2808-2811delACAA[16]。见表4。
表4 不同国家卵巢癌患者BRCA1/2变异比较
Table 4 Comparison of ovarian cancer BRCA1/2 gene variants in different countries
StudiesBRCA1BRCA2ReferenceThis Article Datac.5470-5477delc.981-982delc.6373-6374insA-Arabc.1140 dupgc.5530delc.5095-[9]Turkeyc.2800C>T-[10]South Koreac.3627insAc.7480C>T[11]Italyc.5266dupCc.6313delA[12]Canadac.5266dupCc.1593dup[13]Argentinac.5266dupCc.1138delA[14]Brazilc.5266dupCc.3331-3334delCAAG c.211A > Gc.5946delT c.640 - 6409 delCTTAA[15]Colombiac.3331- 3334delCAAGc.5123C >c.2808 - 2811 delACAA[16]
讨 论
在310例卵巢癌患者中,BRCA1/2基因突变率为28.1%,BRCA1基因突变率为20.1%,BRCA2基因突变率为8.0%,BRCA1基因突变率高于BRCA2基因突变率,移码突变、无义突变、错义突变是BRCA1/2突变的主要类型,约占97.7%,与首个针对中国卵巢癌患者BRCA1/2基因突变的国家多中心研究分析相似(28.5%)[17-18]。BRCA1的c.5470-547del突变是中国研究的热点突变,中国突变频率最高,其次是c.981-982del[19]。本研究也不例外,在c.5470-5477del中有9个突变,在c.981-982del中有7个突变。在BRCA2突变中,以c.6373-6374insA突变为主,与3109C>T和c.7480C>T不一致,这可能是遗传过程中南北差异或基因重组所致。研究表明,德国犹太人卵巢癌患者BRCA基因突变率最高,约为30%~40%;日本最近一项关于卵巢癌BRCA突变研究显示,卵巢癌BRCA1/2突变率高达48.5%;土耳其为31.6%,沙特为29.2%,阿根廷为24.1%,韩国和泰国较低,分别为16.5%和17.3%[20-21]。由此可见,卵巢癌BRCA1/2基因突变率在不同国家存在差异。
卵巢癌BRCA基因突变存在种族和地区差异。在这项研究中,分别包括来自德国犹太人、亚洲、欧洲、北美和南美的一些国家。虽然南美的巴西和哥伦比亚都有c.3331-3334delCAAG突变,但它们并不相同,巴西最常见的BRCA1变异体为c.5266dupC, 而在BRCA1突变体中,c.5266dupC常见于欧洲的波兰和意大利,北美的加拿大,南美的阿根廷和巴西[22]。中国东部地区部分卵巢癌患者BRCA1基因变异体与中国其他省份相同,但BRCA2基因突变最常见的突变为c.6373-6374insA。在BRCA基因突变中,不同国家卵巢癌患者治疗疗效也各不相同,阿拉伯BRCA基因突变卵巢癌患者一线治疗完全缓解率为92%,复发率为84%,韩国BRCA基因突变卵巢癌患者复发率为60.8%;中国BRCA基因突变携带者为1/300,德系犹太人BRCA基因突变携带者为1/40~50,此差异与BRCA基因突变体差异可能存在一定关系[23-24]。
1 Artioli G,Giannone G,Valabrega G,et al.Characteristics and outcome of BRCA mutated epithelial ovarian cancer patients in Italy:A retrospective multicenter study(MITO 21).Gynecol Oncol,2021,161:755-761.
2 Varol U,Kucukzeybek Y,Alacacioglu A,et al.BRCA genes:BRCA 1 and BRCA 2.J BUON,2018,23:862-866.
3 Li K,Zeng J,Zhang M,et al.BRCA variants do not increase the risk of adverse reactions in patients with ovarian cancer:A single-center real-world study.Front Oncol,2022,12:807748.
4 Cardoso FC,Goncalves S,Mele PG,et al.BRCA1 and BRCA2 mutations and clinical interpretation in 398 ovarian cancer patients:comparison with breast cancer variants in a similar population.Hum Genomics,2018:39.
5 Nguyen-Dumont T,Karpinski P,Sasiadek MM,et al.Genetic testing in Poland and Ukraine:should comprehensive germline testing of BRCA1 and BRCA2 be recommended for women with breast and ovarian cancer.Genet Res(Camb),2020,102:e6.
6 Talwar V,Rauthan A.BRCA mutations:Implications of genetic testing in ovarian cancer.Indian J Cancer,2022,59:S56-S67.
7 Bu H,Chen J,Li Q,et al.BRCA mutation frequency and clinical features of ovarian cancer patients:A report from a Chinese study group.J Obstet Gynaecol Res,2019,45:2267-2274.
8 Sekine M,Enomoto T,Arai M,et al.Differences in age at diagnosis of ovarian cancer for each BRCA mutation type in Japan:optimal timing to carry out risk-reducing salpingo-oophorectomy.J Gynecol Oncol,2022,33:e46.
9 Agha N,Alshamsan B,Al-Farsi S,et al.Assessing frequency and clinical outcomes of BRCA mutated ovarian cancer in Saudi women.BMC Cancer,2022,22:18.
10 Cotrim DP,Ribeiro A,Paixão D,et al.Prevalence of BRCA1 and BRCA2 pathogenic and likely pathogenic variants in non-selected ovarian carcinoma patients in Brazil.BMC Cancer,2019,19:4.
11 Kwon BS,Byun JM,Lee HJ,et al.Clinical and genetic characteristics of BRCA1/2 mutation in Korean ovarian cancer patients:A Multicenter study and literature review.Cancer Res Treat,2019,51:941-950.
12 Foglietta J,Ludovini V,Bianconi F,et al.Prevalence and spectrum of BRCA germline variants in central Italian high risk or familial breast/ovarian cancer patients:A monocentric study.Genes(Basel),2020,11:925.
13 Castéra L,Krieger S,Rousselin A,et al.Next-generation sequencing for the diagnosis of hereditary breast and ovarian cancer using genomic capture targeting multiple candidate genes.Eur J Hum Genet,2014,22:1305-1313.
14 Martin CA,Suárez Villasmil L,Sembaj A,et al.[Clinical characteristics of patients with breast and / or ovarian cancer with mutations in the BRCA1 and BRCA2 genes in Córdoba,argentina].Rev Fac Cien Med Univ Nac Cordoba.2022,79:228-234.
15 Sunar V,Korkmaz V,Topcu V,et al.Frequency of germline BRCA1/2 mutations and association with clinicopathological characteristics in Turkish women with epithelial ovarian cancer.Asia Pac J Clin Oncol,2022,18:84-92.
16 Jara L,Morales S,de Mayo T,et al.Mutations in BRCA1,BRCA2 and other breast and ovarian cancer susceptibility genes in Central and south American populations.Biol Res,2017,50:35.
17 Wu X,Wu L,Kong B,et al.The first nationwide multicenter prevalence study of germline BRCA1 and BRCA2 mutations in Chinese Ovarian cancer patients.Int J Gynecol Cancer,2017,27:1650-1657.
18 Pan Z,Xie X.BRCA mutations in the manifestation and treatment of ovarian cancer.Oncotarget,2017,8:97657-97670.
19 Li A,Xie R,Zhi Q,et al.BRCA germline mutations in an unselected nationwide cohort of Chinese patients with ovarian cancer and healthy controls.Gynecol Oncol,2018,151:145-152.
20 Sekine M,Nishino K,Enomoto T.Differences in ovarian and other cancers risks by population and brca mutation location.Genes(Basel),2021,12:1050.
21 Alhuqail AJ,Alzahrani A,Almubarak H,et al.High prevalence of deleterious BRCA1 and BRCA2 germline mutations in arab breast and ovarian cancer patients.Breast Cancer Res Treat,2018,168:695-702.
22 Shaw T,Chan SH,Teo JX,et al.Investigation into the origins of an ancient BRCA1 founder mutation identified among Chinese families in Singapore.Int J Cancer,2021,148:637-645.
23 Kwong A,Shin VY,Ho JC,et al.Comprehensive spectrum of BRCA1 and BRCA2 deleterious mutations in breast cancer in Asian countries.J Med Genet,2016,53:15-23.
24 Kim SI,Lee M,Kim HS,et al.Effect of BRCA mutational status on survival outcome in advanced-stage high-grade serous ovarian cancer.J Ovarian Res,2019,12:40.