随着生育年龄推迟及辅助生殖技术应用增加[1],双胎出生率呈上升趋势,如美国双胎出生率从1980年的18.9‰上升到2006年的32.1‰[2]。双胎妊娠为高危妊娠,不良妊娠结局发生风险高于单胎妊娠[3]。双胎妊娠早产发生率高于50%[4-5],胎死宫内的发生率高达3.7%~6.8%[6]。因此,双胎妊娠围产期的监测尤为重要。超声检查是监测胎儿宫内生长发育情况的主要手段,常用体格发育生物学参数包括双顶径、头围、腹围和股骨长[7]。可靠的超声生物学参数参考值范围是识别胎儿病理性生长发育不良的重要前提[8],但目前临床上多应用单胎妊娠胎儿参考值范围评价双胎妊娠胎儿生长发育情况[9],尚缺乏针对国内人群的双胎特异性胎儿体格发育超声生物学参数参考值范围。
国外研究表明[9-13],双胎妊娠胎儿体格发育超声生物学参数参考值范围上限和下限均低于单胎妊娠胎儿,双绒毛膜双胎胎儿超声生物学参数参考值范围上限和下限均高于单绒毛膜双胎胎儿。国内有研究[14-15]比较了单胎胎儿和双胎胎儿超声生物学参数,发现双胎胎儿各生物学参数在孕晚期的增长速率明显低于单胎,但并未给出参考值范围。国内另一研究[16]给出了双胎妊娠胎儿孕28~34周超声生物学参数参考值范围,但该研究样本量相对较小,未经统计模型拟合,也未考虑不同绒毛膜性双胎之间的差异。
本研究旨在利用较大规模双胎胎儿超声检查数据,采用多水平样条回归方法,建立绒毛膜特异性双胎胎儿体格发育超声生物学参数的参考值范围,为双胎胎儿宫内生长发育监测及临床诊疗提供参考。
对象与方法
一、对象
研究对象为2007年至2017年在北京大学第三医院产检并分娩的双胎妊娠胎儿。纳入标准:(1)双胎均活胎;(2)夫妇双方均为中国国籍;(3)核对孕周准确;(4)绒毛膜性明确。排除标准:(1)胎儿结构畸形或染色体异常;(2)单绒毛膜单羊膜囊双胎;(3)分娩孕周小于34周;(4)单绒毛膜双胎特殊并发症,如双胎输血综合征等。
研究最初收集符合纳入标准的双胎1 247对,剔除分娩孕周小于34周(144对)、胎儿结构畸形或染色体异常(10对)、单绒毛膜单羊膜囊(32对)、单绒毛膜双胎孕期特殊并发症(74对)、超声数据不完整(104对)对象后,最终纳入883对双胎,其中双绒毛膜双胎704对(79.7%),单绒毛膜双胎179对(20.3%)。883对双胎共接受3 185次超声测量(即6 370条超声检查记录),检查孕周分布在16~37周。
二、方法
1. 研究设计:研究依托国家重点研发计划项目“高龄产妇妊娠期并发症防治策略研究”双胎专项课题而开展。研究数据来源于北京大学第三医院,主体上包括双胎妊娠孕妇妊娠期超声检查数据及分娩数据。超声检查数据包括检查孕周,各生物学超声参数(双顶径、头围、腹围、股骨长)等变量,超声医师均按标准化测量规范实施测量;分娩数据包括孕妇年龄、分娩孕周、绒毛膜性、胎儿性别、出生体重等变量。通过拟合多水平样条模型,构建双胎妊娠胎儿孕中晚期双顶径、头围、腹围、股骨长的参考值范围。
2. 统计学处理:研究按照绒毛膜性分层,建立四个参数参考值范围。为避免极端值影响,剔除了各孕周四个参数的极端值[(<下四分位数值-3)×四分位数间距,或(>上四分位数值+3)×四分位数间距]。为改善方差齐性,将各生物学参数做了对数转换。因同一孕妇两个胎儿及同一胎儿多次超声测量存在自相关性,研究采用多水平样条回归模型拟合数据,测量值为水平1变量,胎儿为水平2变量(随机截距),孕妇为水平3变量(随机截距和随机斜率),样条可选节点设为0~3个,采用赤池信息准则[17]确定最优模型,利用最优模型估计各参数各孕周均值和标准差,进而计算各参数各孕周3%、10%、50%、90%和97%分位数,并将10%分位数作为参考值范围的下限,90%分位数作为参考值范围的上限。
结 果
双绒毛膜双胎妊娠孕妇年龄高于单绒毛膜双胎妊娠孕妇,双绒毛膜双胎妊娠辅助生殖技术助孕者占比(40%)显著高于单绒毛膜双胎妊娠(10%),双绒毛膜双胎平均分娩孕周和平均出生体重均显著高于单绒毛膜双胎,差异均有统计学意义。双绒毛膜双胎和单绒毛膜双胎胎儿性别构成相似,男性胎儿依次为51.2%和49.4%。单绒毛膜双胎妊娠孕妇妊娠期高血压疾病发病率略高于双绒毛膜双胎妊娠孕妇,而双绒毛膜双胎妊娠孕妇妊娠期糖尿病发病率略高于单绒毛膜双胎妊娠孕妇,但差异均无统计学差异。单绒毛膜双胎妊娠孕妇中位超声检查次数显著高于双绒毛膜孕妇,差异有统计学意义。见表1。
表1 研究对象基本情况表(n=883对双胎)
Table 1 Baseline characteristics of twin pregnancy (n=883)
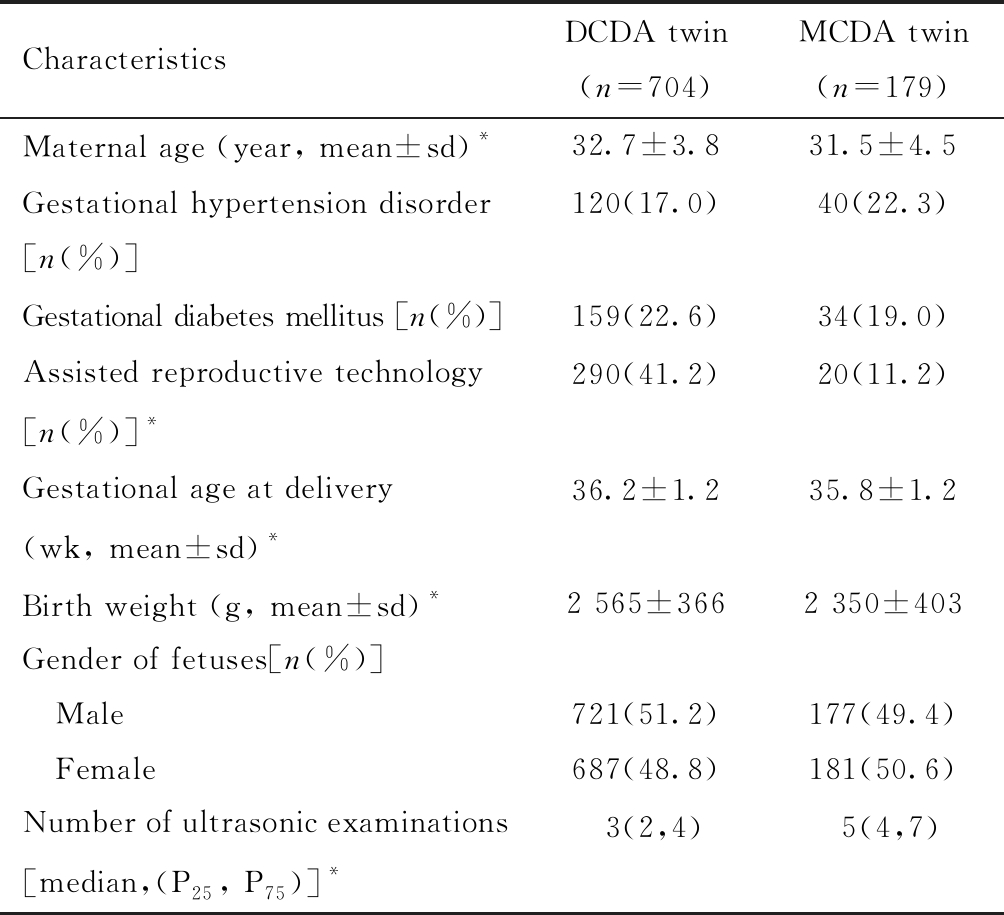
CharacteristicsDCDA twin(n=704)MCDA twin(n=179)Maternal age (year, mean±sd)*32.7±3.831.5±4.5Gestational hypertension disorder[n(%)]120(17.0)40(22.3)Gestational diabetes mellitus [n(%)]159(22.6)34(19.0)Assisted reproductive technology[n(%)]*290(41.2)20(11.2)Gestational age at delivery (wk, mean±sd)*36.2±1.235.8±1.2Birth weight (g, mean±sd) *2 565±3662 350±403Gender of fetuses[n(%)] Male721(51.2)177(49.4) Female687(48.8)181(50.6)Number of ultrasonic examinations[median,(P25, P75)] *3(2,4)5(4,7)
*P<0.05; dichorionic diamniotic(DCDA); monochorionic diamniotic(MCDA)
图1展示了不同绒毛膜性胎儿双顶径、头围、腹围和股骨长参考值范围。由图可见,不管双绒毛膜双胎还是单绒毛膜双胎,各参数总体上均随着孕周增加而增大,双顶径、头围和股骨长的增长速率在孕晚期有所下降,腹围增长速率变化不明显,各参数参考值范围宽度(即上限与下限间距)随着孕周增加而增大。双绒毛膜双胎四个参数参考值范围上下限总体上略高于单绒毛膜双胎。具体而言,二者90%分位数即上限几乎重叠,50%分位数略有差异,而双绒毛膜双胎10%分位数即下限明显高于单绒毛膜双胎;双绒毛膜双胎与单绒毛膜双胎四个参数在孕16~20周时差距较大,20~28周差距较小,28周之后差距随孕周增加而增大;双绒毛膜双胎和单绒毛膜双胎双顶径和头围相差较小,腹围和股骨长相差较大。
表2~表5展示了不同绒毛膜性胎儿孕16~37周四个超声生物学参数90%分位数(参考值范围上限)、50%分位数和10%分位数(参考值范围下限)具体数值,同时还给出了3%和97%分位数。

![]()
*dichorionic diamniotic(DCDA); **monochorionic diamniotic(MCDA)
图1 双胎妊娠胎儿孕中晚期双顶径(BPD)、头围(HC)、腹围(AC)、股骨长(FL)第10%、50%和90%分位数线
Figure 1 The 10th, 50th and 90th percentiles of:biparietal diameter (BPD), head circumference (HC), abdominal circumference (AC),and femur length (FL) measurements in the second- and third-trimester of twin pregnancy
表2 双胎妊娠胎儿孕中晚期超声双顶径参考值范围(cm)
Table 2 Fetal reference range of biparietal diameter in the second- and third-trimester of twin pregnancy (cm)
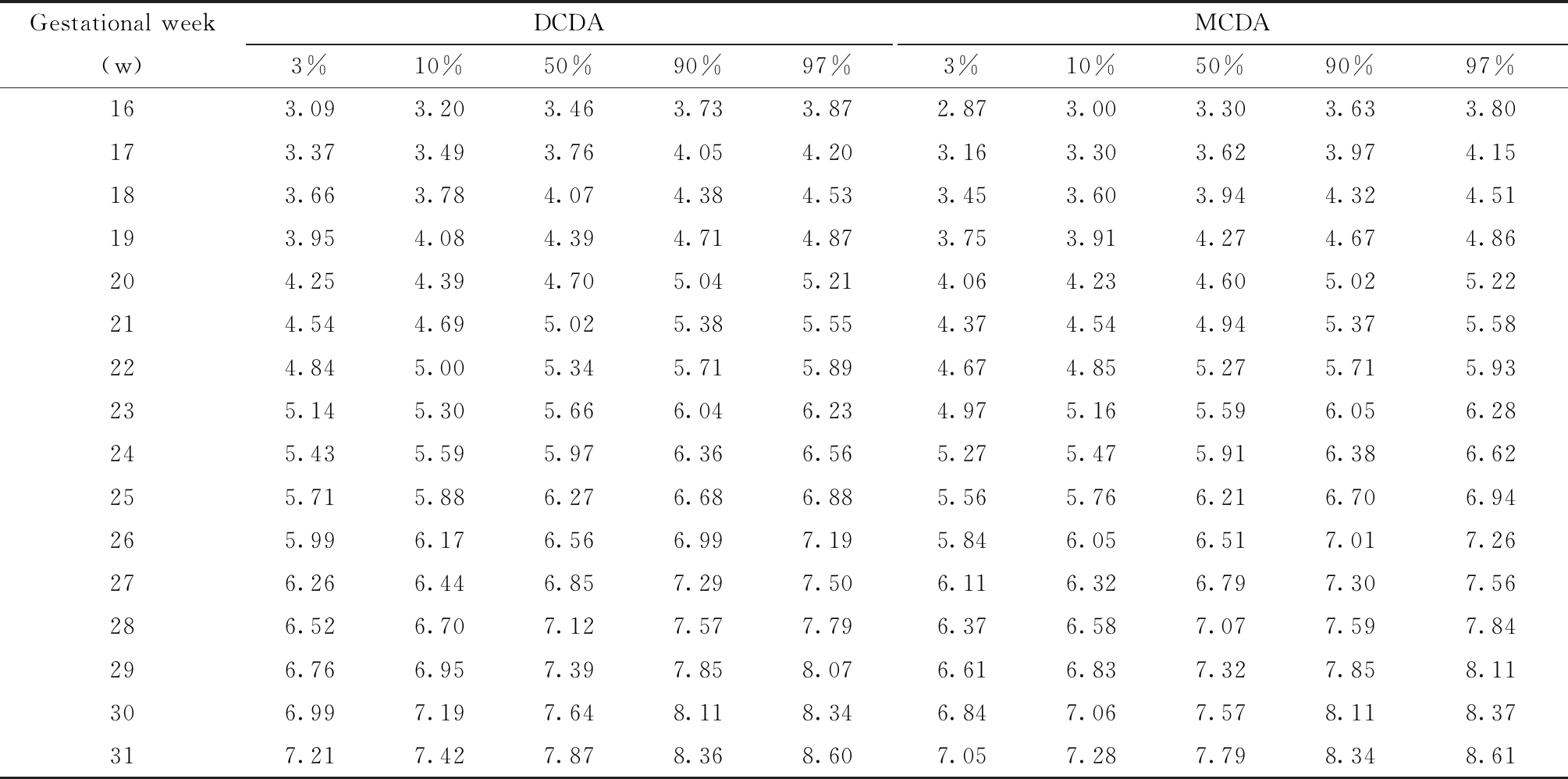
Gestational week(w)DCDA3%10%50%90%97%MCDA3%10%50%90%97%163.093.203.463.733.872.873.003.303.633.80173.373.493.764.054.203.163.303.623.974.15183.663.784.074.384.533.453.603.944.324.51193.954.084.394.714.873.753.914.274.674.86204.254.394.705.045.214.064.234.605.025.22214.544.695.025.385.554.374.544.945.375.58224.845.005.345.715.894.674.855.275.715.93235.145.305.666.046.234.975.165.596.056.28245.435.595.976.366.565.275.475.916.386.62255.715.886.276.686.885.565.766.216.706.94265.996.176.566.997.195.846.056.517.017.26276.266.446.857.297.506.116.326.797.307.56286.526.707.127.577.796.376.587.077.597.84296.766.957.397.858.076.616.837.327.858.11306.997.197.648.118.346.847.067.578.118.37317.217.427.878.368.607.057.287.798.348.61
表2(续)
Gestational week(w)DCDA3%10%50%90%97%MCDA3%10%50%90%97%327.427.638.108.608.847.257.488.018.578.84337.617.828.318.829.077.437.678.218.789.06347.788.008.509.039.287.607.858.398.979.26357.948.178.689.229.497.768.018.569.169.45368.098.328.859.409.687.908.158.729.339.63378.228.469.009.579.858.038.298.879.499.80
Dichorionic diamniotic(DCDA); Monochorionic diamniotic(MCDA)
表3 双胎妊娠胎儿孕中晚期超声头围参考值范围(cm)
Table 3 Fetal reference range of head circumference in the second- and third-trimester of twin pregnancy (cm)

Gestational week(w)DCDA3%10%50%90%97%MCDA3%10%50%90%97%1611.3311.6912.4913.3613.7810.4910.9211.8912.9613.491712.3912.7713.6314.5414.9911.5712.0313.0714.2014.761813.4813.8814.7915.7516.2212.6813.1714.2715.4616.051914.5915.0115.9616.9617.4513.8214.3315.4816.7317.342015.7016.1417.1318.1818.6914.9615.5016.7018.0018.642116.8217.2818.3019.3919.9216.1116.6617.9119.2519.922217.9318.4019.4620.5821.1317.2517.8219.1120.4921.172319.0219.5120.6121.7622.3218.3718.9620.2821.7022.402420.0920.6021.7222.9123.4819.4720.0721.4322.8723.582521.1421.6622.8124.0224.6120.5321.1522.5324.0024.732622.1422.6823.8625.1025.7021.5622.1923.5925.0925.822723.1123.6524.8626.1326.7522.5423.1824.6026.1226.852824.0324.5925.8227.1227.7423.4824.1225.5627.0927.842924.9125.4726.7328.0528.6924.3525.0126.4728.0128.763025.7326.3127.5928.9429.5925.1825.8427.3128.8729.633126.4927.0928.4029.7830.4425.9426.6128.1129.6830.453227.2127.8129.1630.5631.2526.6527.3328.8430.4431.213327.8628.4929.8631.3032.0027.3027.9929.5331.1531.933428.4729.1130.5231.9932.7127.9028.6030.1631.8132.613529.0229.6831.1332.6433.3828.4529.1630.7632.4433.253629.5330.2031.6933.2534.0128.9529.6831.3133.0333.873729.9930.6832.2233.8334.6129.4130.1631.8333.6034.46
Dichorionic diamniotic(DCDA); Monochorionic diamniotic(MCDA)
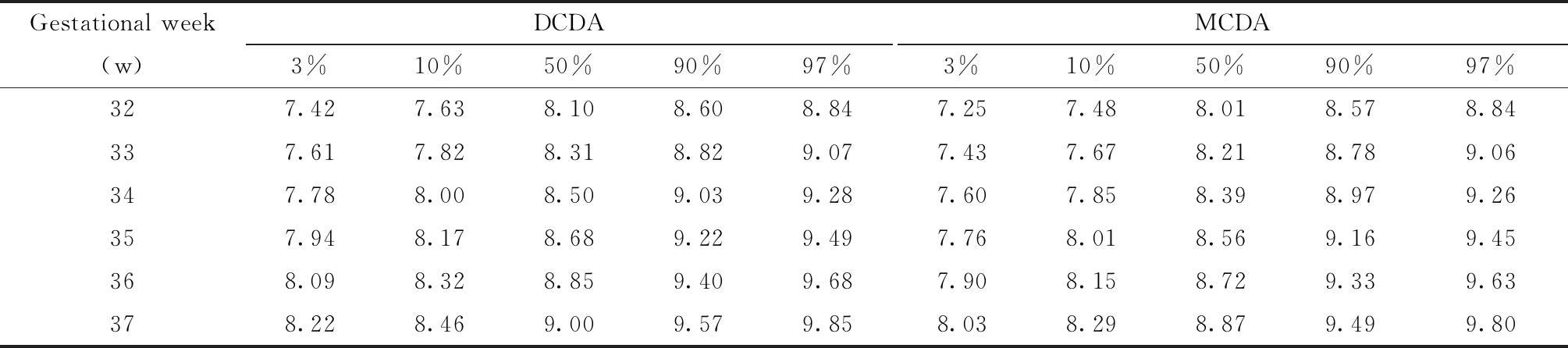
表4 双胎妊娠胎儿孕中晚期超声腹围参考值范围(cm)
Table 4 Fetal reference range of abdominal circumference in the second- and third-trimester of twin pregnancy (cm)
Gestational week(w)DCDA3%10%50%90%97%MCDA3%10%50%90%97%169.299.6610.5011.4011.868.348.779.7810.9011.471710.2410.6311.5312.5012.999.359.8310.9212.1412.761811.2111.6312.5913.6314.1510.3910.9012.0813.4014.061912.2012.6513.6714.7815.3211.4311.9813.2514.6515.352013.2113.6914.7715.9416.5112.4813.0614.4115.8916.632114.2314.7315.8717.1017.7113.5214.1315.5517.1117.892215.2515.7816.9818.2718.9014.5415.1916.6718.3019.11
表4(续)
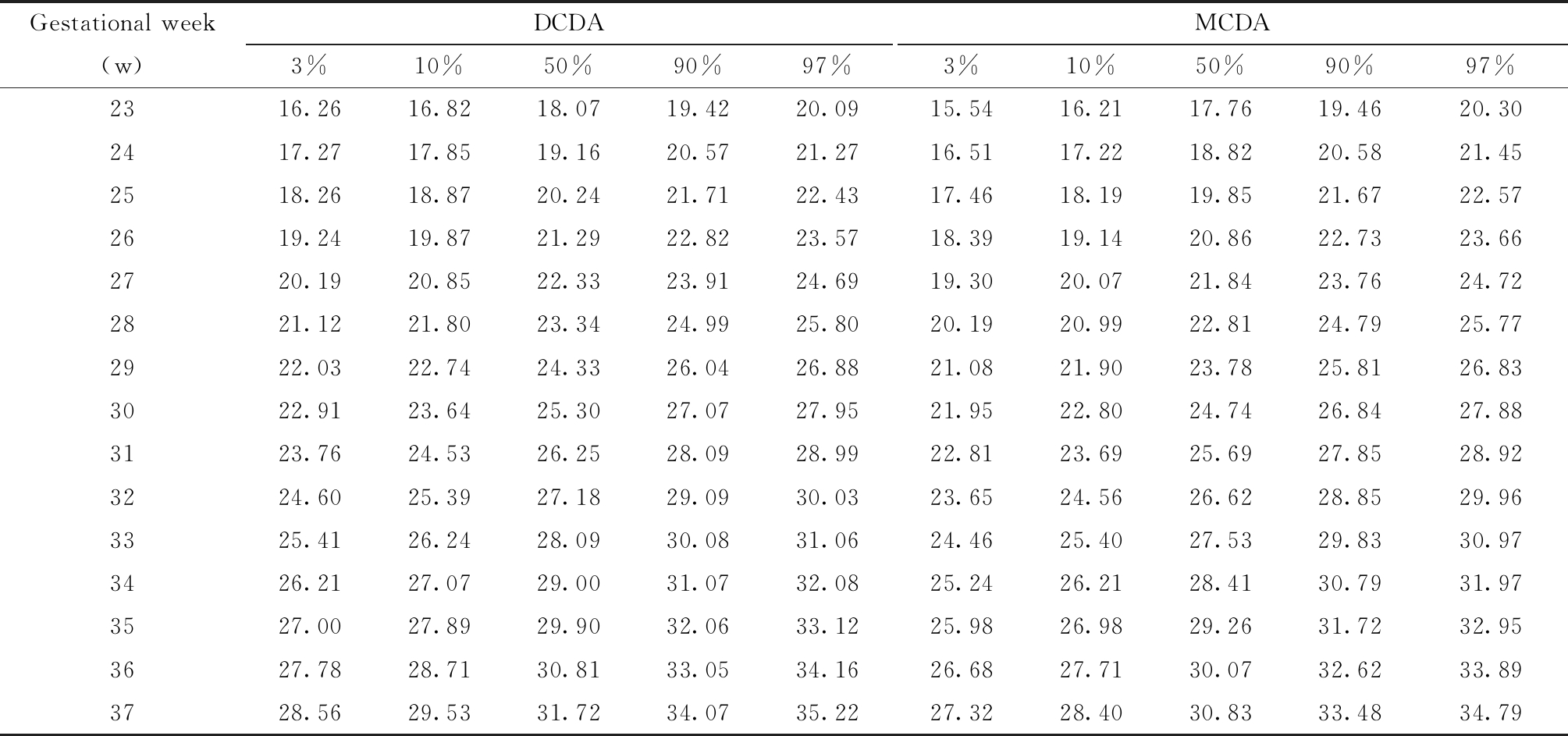
Gestational week(w)DCDA3%10%50%90%97%MCDA3%10%50%90%97%2316.2616.8218.0719.4220.0915.5416.2117.7619.4620.302417.2717.8519.1620.5721.2716.5117.2218.8220.5821.452518.2618.8720.2421.7122.4317.4618.1919.8521.6722.572619.2419.8721.2922.8223.5718.3919.1420.8622.7323.662720.1920.8522.3323.9124.6919.3020.0721.8423.7624.722821.1221.8023.3424.9925.8020.1920.9922.8124.7925.772922.0322.7424.3326.0426.8821.0821.9023.7825.8126.833022.9123.6425.3027.0727.9521.9522.8024.7426.8427.883123.7624.5326.2528.0928.9922.8123.6925.6927.8528.923224.6025.3927.1829.0930.0323.6524.5626.6228.8529.963325.4126.2428.0930.0831.0624.4625.4027.5329.8330.973426.2127.0729.0031.0732.0825.2426.2128.4130.7931.973527.0027.8929.9032.0633.1225.9826.9829.2631.7232.953627.7828.7130.8133.0534.1626.6827.7130.0732.6233.893728.5629.5331.7234.0735.2227.3228.4030.8333.4834.79
Dichorionic diamniotic(DCDA); Monochorionic diamniotic(MCDA)
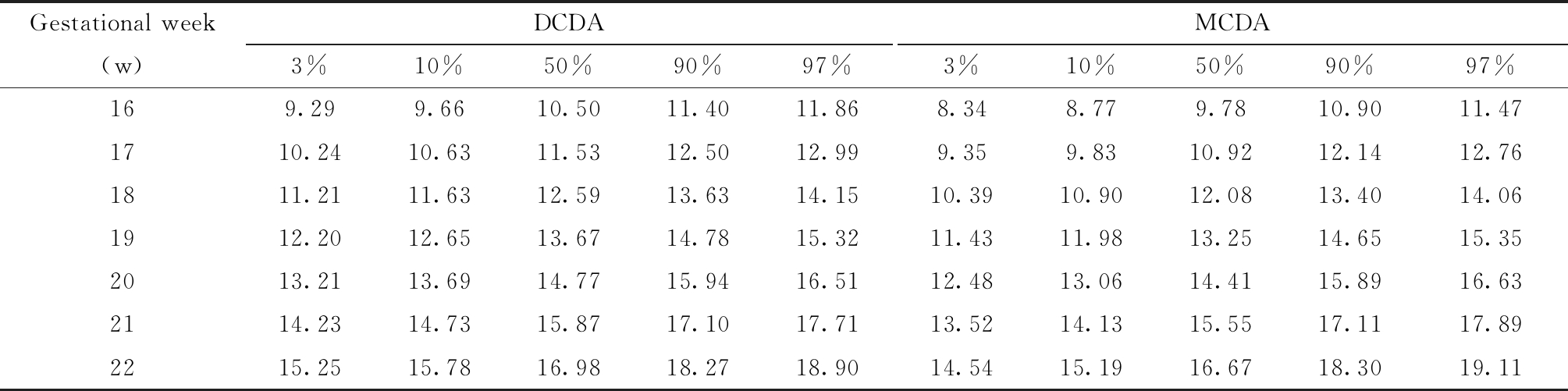
表5 双胎妊娠胎儿孕中晚期超声股骨长参考值范围(cm)
Table 5 Fetal reference range of femur length in the second- and third-trimester of twin pregnancy (cm)
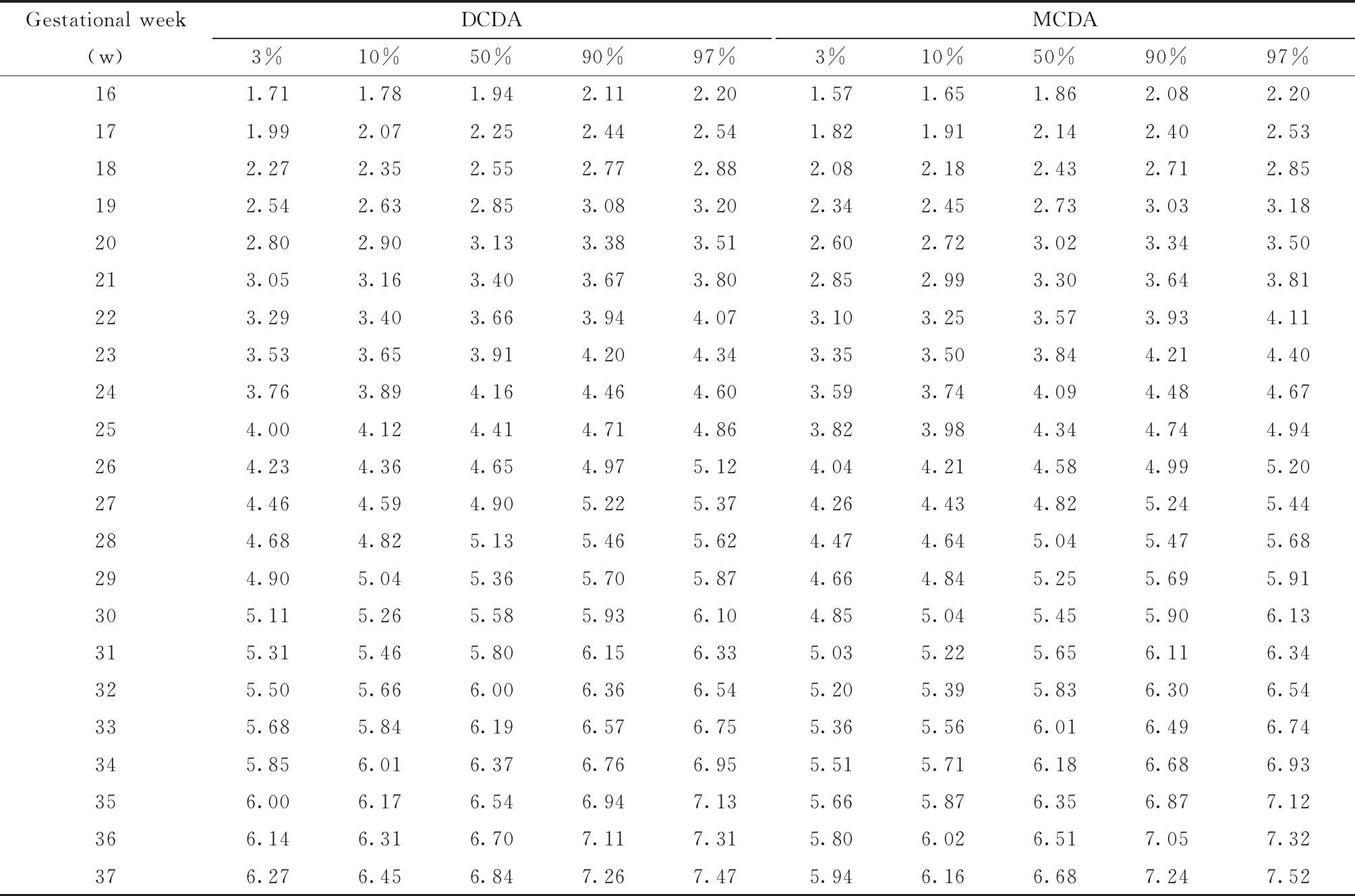
Gestational week(w)DCDA3%10%50%90%97%MCDA3%10%50%90%97%161.711.781.942.112.201.571.651.862.082.20171.992.072.252.442.541.821.912.142.402.53182.272.352.552.772.882.082.182.432.712.85192.542.632.853.083.202.342.452.733.033.18202.802.903.133.383.512.602.723.023.343.50213.053.163.403.673.802.852.993.303.643.81223.293.403.663.944.073.103.253.573.934.11233.533.653.914.204.343.353.503.844.214.40243.763.894.164.464.603.593.744.094.484.67254.004.124.414.714.863.823.984.344.744.94264.234.364.654.975.124.044.214.584.995.20274.464.594.905.225.374.264.434.825.245.44284.684.825.135.465.624.474.645.045.475.68294.905.045.365.705.874.664.845.255.695.91305.115.265.585.936.104.855.045.455.906.13315.315.465.806.156.335.035.225.656.116.34325.505.666.006.366.545.205.395.836.306.54335.685.846.196.576.755.365.566.016.496.74345.856.016.376.766.955.515.716.186.686.93356.006.176.546.947.135.665.876.356.877.12366.146.316.707.117.315.806.026.517.057.32376.276.456.847.267.475.946.166.687.247.52
Dichorionic diamniotic(DCDA); Monochorionic diamniotic(MCDA)
表6显示了孕16~37周实际测量值低于本研究所建立的参考值下限人次占比,以及低于既往研究建立的单胎妊娠胎儿四个参数参考值范围[8]下限人次占比。双绒毛膜双胎四个参数实际测量值低于本研究所建立的参考值范围下限人次占比为11.8%、12.9%、12.0%和12.1%,单绒毛膜双胎四个参数实际测量值低于本研究所建立的参考值范围下限人次占比为10.4%、10.4%、10.3%和10.6%,两类胎儿四个参数实际测量值低于单胎妊娠胎儿参考值范围下限人次分别占25.4%~39.0%(较双绒毛膜双胎高13.6~27.0个百分点)和32.8%~50.3%(较单绒毛膜双胎高22.4~40.0个百分点)。
表6 不同参考值范围下各周超声检查值低于10%分位数人次占比(%)
Table 6 The proportion of ultrasonic measurements under lower limits of different fetal reference range(%)
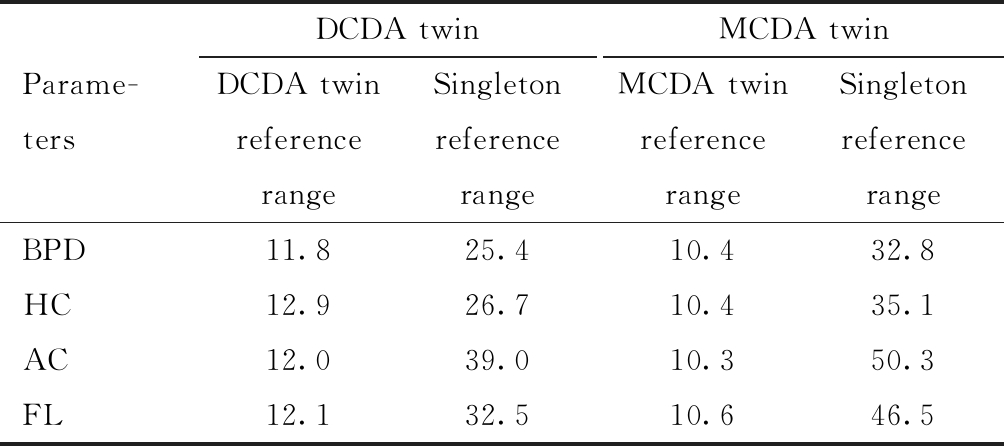
Parame-tersDCDA twinDCDA twin reference rangeSingleton reference rangeMCDA twinMCDA twin reference rangeSingleton reference rangeBPD11.825.410.432.8HC12.926.710.435.1AC12.039.010.350.3FL12.132.510.646.5
Dichorionic diamniotic(DCDA); Monochorionic diamniotic(MCDA)
讨 论
胎儿宫内生长发育情况是围产保健对胎儿监测的重要内容,双顶径、头围、腹围和股骨长是评价胎儿宫内发育情况的重要指标,相应参考值范围可作为识别胎儿发育异常的重要依据。本研究利用双胎妊娠超声检查数据,构建了绒毛膜特异性双胎胎儿孕16~37周四个体格发育超声生物学参数参考值范围。同文献报道的单胎胎儿超声生物学参数参考值范围相比,本研究所建立的参考值范围能使双绒毛膜双胎胎儿四个超声生物学参数可疑发育不良(即低于参考值范围下限)检出比例降低13.6~27.0个百分点,能使单绒毛膜双胎胎儿四个超声生物学参数可疑发育不良检出比例降低22.4~40.0个百分点,预期能显著减少过度诊断引发的心理负担及不必要的临床干预。
受营养供给和生长空间限制,双胎妊娠胎儿妊娠晚期生长发育速度低于单胎。意大利、英国、美国等多个研究团队建立了双胎妊娠特异性超声生物学参数参考值范围[9, 13, 18],并发现双胎妊娠特异性参考值范围有助于大幅减少胎儿可疑发育不良比例。单绒毛膜双胎两个胎儿共用一个胎盘,胎儿生长速率同比低于双绒毛膜双胎,鉴于此多数研究按照绒毛膜性分层,分别建立了双绒毛膜双胎和单绒毛膜双胎超声生物学参数参考值范围。通过比较分析,本研究发现中国人群双绒毛膜双胎与单绒毛膜双胎、双胎妊娠胎儿与单胎妊娠胎儿在体格发育方面的差异特征与国外研究相近。但值得注意的是,不同种族胎儿体格发育情况可能存在明显差异,不宜将国外双胎妊娠胎儿超声生物学参数参考值范围直接用于评价中国双胎妊娠胎儿体格发育情况。例如,英国学者开展的参考值范围研究[13]显示,双绒毛膜双胎孕20周双顶径、头围、腹围、股骨长的10%分位数依次为4.54 cm、16.46 cm、13.87 cm、2.95 cm,而本研究双绒毛膜双胎四个参数10%分位数依次为4.39 cm、16.14 cm、13.69 cm、2.90 cm(表2~表5);英国研究单绒毛膜双胎孕20周四个参数10%分位数依次为4.49 cm、16.19 cm、13.59 cm、2.86 cm,而本研究单绒毛膜双胎四个参数10%分位数依次为4.23 cm、15.50 cm、13.06 cm、2.72 cm(表2~表5)。不同国家不同种族双胎胎儿生长发育差异可能与遗传、地理、饮食习惯等多种因素有关[19]。
本研究利用较大规模双胎胎儿超声检查数据,首次针对中国人群采用国际主流统计建模方法,建立了绒毛膜特异性双胎孕中晚期体格发育超声生物学参数参考值范围,该参考值范围在一定程度上填补了国内在相关领域的空白,具有较高临床参考价值。本研究所用资料源自临床超声数据,不同超声医师针对四个超声生物学参数的测量操作可能存在一定差异,但所有超声医师均按标准化测量规范实施测量,预期超声医师之间的测量误差不会对研究结果造成实质影响。本研究在选取对象时排除了可能影响胎儿体格发育的严重疾病或并发症(如死胎死产、小于34周早期早产、胎儿结构畸形和染色体异常等),同时还剔除了极端值,表明建模人群主体上为体格发育相对正常的双胎胎儿。鉴于此,尽管本研究为单中心研究,但所建立的超声生物学参数参考值范围仍应具有较好适用性,尤其是双绒毛膜双胎,建模所用样本较大,相应参考值范围稳定性可能更高,值得验证与推广。
1 Piro E,Schierz IAM,Serra G,et al.Growth patterns and associated risk factors of congenital malformations in twins.Ital J Pediatr,2020,46:73.
2 Chauhan SP,Scardo JA,Hayes E,et al.Twins:Prevalence,problems,and preterm births.Am J Obstet Gynecol,2010,203:305-315.
3 张舒沁,王静,魏瑗.双胎妊娠的孕期管理.中国实用妇科与产科杂志,2020,36:114-117.
4 Martin JA,Hamilton BE,Osterman MJ,et al.Births:Final data for 2013. Natl Vital Stat Rep,2015,64:1-65.
5 蒋芳,高劲松,钟逸锋,等.北京协和医院25年早产状况的调查.中国医学科学院学报,2016,38:528-533.
6 Blickstein I,Perlman S.Single fetal death in twin gestations.J Perinat Med,2013,41:65-69.
7 Rasmussen S.Charts to assess fetal wellbeing.Ultrasound Obstet Gynecol,2011,37:2-5.
8 张一休.中国胎儿超声生物学参数生长曲线及参考范围的研究与建立.北京协和医学院,2019.
9 Ghi T,Prefumo F,Fichera A,et al.Development of customized fetal growth charts in twins.Am J Obstet Gynecol,2017,216:514.e1-514.e17.
10 Leroy B,Lefort F,Neveu P,et al.Intrauterine growth charts for twin fetuses.Acta Genet Med Gemellol (Roma),1982,31:199-206.
11 Grennert L,Persson PH,Gennser G.Intrauterine growth of twins judged by bpd measurements.Acta Obstet Gynecol Scand Suppl,1978,78:28-32.
12 Torres X,Bennasar M,Eixarch E,et al.Gender-specific antenatal growth reference charts in monochorionic twins.Fetal Diagn Ther,2018,44:202-209.
13 Stirrup OT,Khalil A,D′antonio F,et al.Fetal growth reference ranges in twin pregnancy:Analysis of the southwest thames obstetric research collaborative (stork) multiple pregnancy cohort.Ultrasound Obstet Gynecol,2015,45:301-307.
14 刘蓉,谭金秀,陈其能.B超监测双胎与单胎中晚期妊娠胎儿生长发育的比较.中国妇幼保健,2007,22:2538-2539.
15 陈安珍.双胎妊娠胎儿发育及适宜分娩孕周的临床研究.中国实用医药,2008,3:1-2.
16 王晶,杨太珠.超声测量晚孕期正常双胎生长参数的初步分析.华西医学,2011,26:1521-1524.
17 Akaike H.A new look at the statistical model identification.IEEE Trans Automat Contr,1974,19:716-723.
18 Grumbach K,Coleman BG,Arger PH,et al.Twin and singleton growth patterns compared using us.Radiology,1986,158:237-241.
19 周莉娜,文卿.单项超声测量指标预测胎儿体重的临床应用.影像技术,2020,32:20-22.