睡眠(sleep)是机体休息的重要方式,有效而充足的睡眠可充分恢复个体的体力、精力,有利于维持人类躯体和心理健康[1]。正常成年人每日推荐睡眠时长7~8 h,包括夜眠与午睡等形式,午睡作为一种对夜眠时长不足的补充形式,可以改善睡眠不足造成的疲劳、焦虑、注意力不集中等症状。尽管睡眠需求可能因年龄和性别而异,但美国国家睡眠基金会建议成人每 24 h睡眠7 h至8 h [2],7 h为每日睡眠最低限。孕晚期妇女因多方面因素导致睡眠不足[3],基于2017年国内五省孕妇睡眠时间横断面调查结果,23.9%的孕妇睡眠时长≤7h[4]。疲劳(fatigue)是一种非特异性症状,文献报道60%的孕晚期妇女存在疲劳[5],而疲劳会直接影响分娩启动时间、持续时间及分娩形式,并导致孕产妇和婴儿出现一系列短期和长期并发症[6]。孕期睡眠不足是孕妇疲劳的原因之一,增加睡眠时间有可能预防、改善或减少孕妇的疲劳[7]。之前的研究多关注孕期午睡[8],而尚未把孕前午睡对疲劳的影响做为关注点。本研究旨在分析孕前午睡与目前夜眠时长对孕妇孕晚期疲劳程度的影响,探讨睡眠在孕晚期疲劳中的作用。
对象与方法
一、对象
本研究采用方便取样法收集样本,连续收集2020年1~12月于厦门大学医学院第二附属医院就诊的妊娠妇女。纳入标准:(1)签署知情同意书;(2)符合国家生育政策;(3)年龄20~40周岁;(4)孕28~42周,孕妇无临产迹象;(5)孕妇无合并症;(6)单胎且胎儿无异常;(7)能够阅读且理解问卷内容。排除标准:(1)不同意参加研究者;(2)临产或已进入产程者;(3)存在妊娠合并症及并发症、合并重大器质性疾病及内分泌系统疾病;(4)具有明确精神病史、智力障碍、药物及酒精滥用者;(5)无法进行沟通交流者;(6)胎儿存在异常者。本研究经厦门大学医学院附属第二医院伦理委员会批准(批件号2020028),符合各项伦理规范。本次研究共招募妊娠晚期490名孕妇,排除3例缺失夜眠时长样本,有效样本487例。孕妇年龄17~43周岁,平均年龄为(29.1±4.1)周岁,孕周28+1~40+6周。参照夜眠时长及孕前是否午睡对研究样本进行分组,分为“夜眠时长(≤7h)+无午睡”组、“夜眠时长(≤7h)+午睡”组、“夜眠时长(>7h) +无午睡”组、“夜眠时长(>7h)+午睡”组4组。
二、方法
1. 资料收集:研究过程中由项目组专职医护人员进行资料收集,签署知情同意书后进行一般资料采集,使用疲劳评定量表(Fatigue Scale-14,FS-14)[9]进行调查研究。一般资料包括年龄、教育程度、孕前午睡与目前夜眠时长、身高、 体重等自然信息,记录部分临床信息,如血压、肝功、血糖等项目。FS-14量表用以评定受试者疲劳程度及特征,该量表含14项是非选择题,每题记1分,题目分为躯体疲劳及脑力疲劳两部分,1~8项反映躯体疲劳,主要评估受试者对疲劳的自我感受及疲劳对机体的直接影响,例如是否疲劳、是否嗜睡、是否力不从心、是否存在肌力下降等;9~14项反映脑力疲劳,主要涉及注意力、思维能力、语言表达能力、记忆力、兴趣爱好等方面。二者分别占8分、6分,总分14分,各部分得分越高则代表该测试部分疲劳越严重。采用FS-14量表量化孕晚期妇女疲劳程度,将得分整理为总分、躯体疲劳得分、脑力疲劳得分三个项目进行分析。
2. 质量控制:所有入组者均已明确知晓研究意义,理解填写内容,问卷不记名,填写完毕后交由调查人员检查完成程度,并补充遗漏项目。使用Epidata 3.1软件双录入数据,确保录入准确。
3. 统计学处理:全部数据应用SPSS 23.0软件进行分析,采用频数、百分率、均数±标准差对妊娠晚期妇女的一般资料进行描述,采用卡方检验、方差分析(ANOVA)进行妊娠末期各组间一般资料的均衡性检验。FS-14总分、躯体疲劳得分、脑力疲劳得分因其设计不存在正态性,不符合正态性分布(P<0.01),对其进行Levene方差齐性检验,符合方差齐性(P>0.1), 采用2(是否午睡)X2(夜眠有效时长是否大于7 h)的组内设计ANOVA分析二者间交互作用,采用协方差分析(ANCOVA)与广义线性模型(GLM)对组间资料进行最小显著差异(LSD)t检验LSD/简单效应分析,使用Graphpad prism 8.0完成作图。所有检验取双尾,P<0.05为差异具有统计学意义。
结 果
一、基本资料的均衡性分析
本次研究有效样本487例,平均身高(159.1±5.2)cm,平均体重(64.6±9.8)kg,孕前BMI值(21.3±3.2)kg/m2,孕后BMI值(25.5±3.4)kg/m2,ALT(15.0±17.4)U/L。参照夜眠时长及孕前是否午睡对研究样本进行分组,组间年龄、孕前BMI差异无统计学意义,教育程度差异有统计学意义。见表1。
二、疲劳评定量表(FS-14)结果分析
由表2、图1可以看出,夜眠时长≤7 h且无午睡组FS-14总分、躯体疲劳得分、脑力疲劳得分三项得分均为最高分,表明该组孕妇最为疲劳,之后是夜眠时长≤7 h且午睡组及夜眠时长>7 h且午睡组,夜眠时长>7 h且无午睡组三项得分为最低分。不论孕前是否午睡,夜眠时长>7 h的组别,其疲劳总分、躯体疲劳得分均较低。FS-14总分、FS-14躯体疲劳得分组间差异有统计学意义, FS-14脑力疲劳得分组间差异没有统计学意义。
三、孕前午睡与不同夜眠时长对孕晚期疲劳程度的影响
ANOVA分析结果表明,在FS总分上,是否午睡主效应不显著(F(1,483)=1.13,P=0.289);夜眠有效时长的主效应达到显著性水平,(F(1,483)=14.44,P=0.000);且两者的交互作用也达到显著性水平(F(2,483)=5.14,P=0.024)。在FS躯体疲劳得分上,是否午睡主效应不显著(F(1,483)=2.41,P=0.121);夜眠有效时长的主效应达到显著性水平,(F(1,483)=18.12,P=0.000);且两者的交互作用也达到显著性水平(F(2,483)=6.46,P=0.011)。在FS脑力疲劳得分上,是否午睡主效应不显著(F(1,483)=0.16,P=0.688);夜眠有效时长的主效应也未达到显著性水平,(F(1,483)=0.78,P=0.378);且两者的交互作用也未能达到显著性水平(F(2,483)=0.27,P=0.601)。进一步简单主效应分析表明,FS-14总分、FS-14躯体疲劳得分组间差异有统计学意义,FS-14脑力疲劳得分组间差异无统计学意义。见表3。
表1 基本资料比较
Table 1 Basic and Demographic characteristics by different sleeping modes
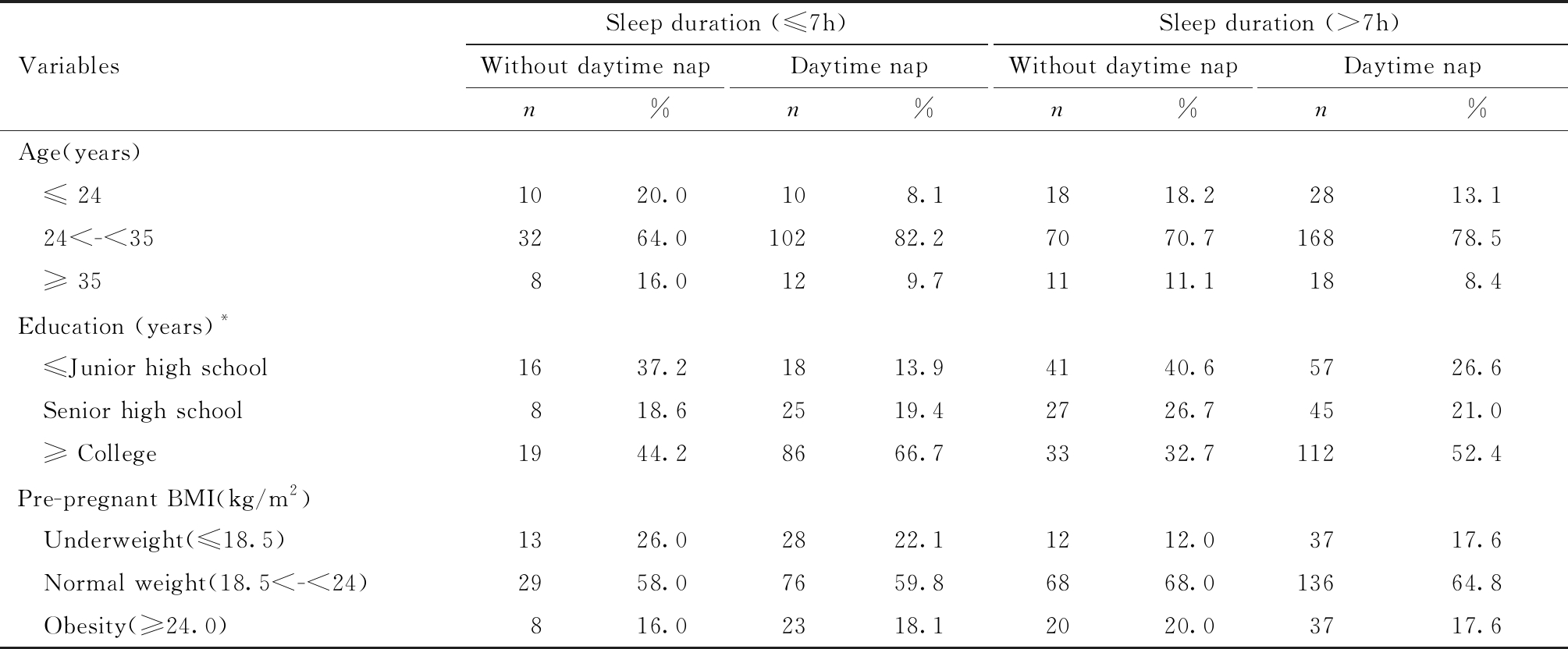
VariablesSleep duration (≤7h)Without daytime napn%Daytime napn%Sleep duration (>7h)Without daytime napn%Daytime napn%Age(years) ≤ 241020.0108.11818.22813.1 24<-<353264.010282.27070.716878.5 ≥ 35816.0129.71111.1188.4Education (years)* ≤Junior high school1637.21813.94140.65726.6 Senior high school818.62519.42726.74521.0 ≥ College1944.28666.73332.711252.4Pre-pregnant BMI(kg/m2) Underweight(≤18.5)1326.02822.11212.03717.6 Normal weight(18.5<-<24)2958.07659.86868.013664.8 Obesity(≥24.0)816.02318.12020.03717.6
*P<0.05
表2 孕晚期FS-14分数得分组间比较![]()
Table 2 FS-14 scores in the third trimester of pregnancy by sleep duration and daytime ![]()
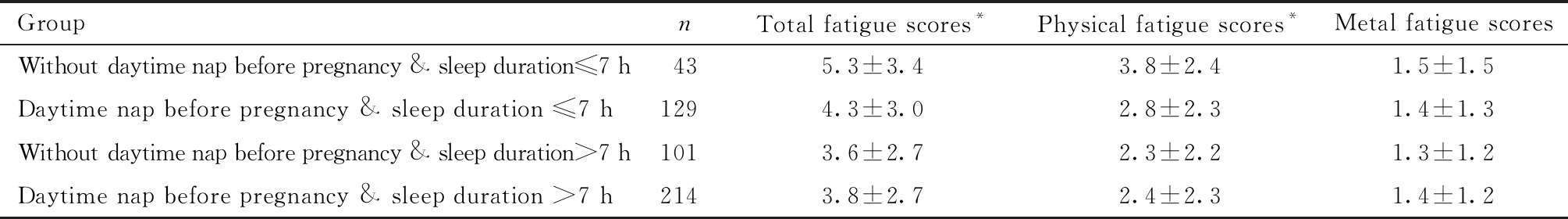
GroupnTotal fatigue scores*Physical fatigue scores*Metal fatigue scoresWithout daytime nap before pregnancy & sleep duration≤7 h435.3±3.43.8±2.41.5±1.5Daytime nap before pregnancy & sleep duration ≤7 h1294.3±3.02.8±2.31.4±1.3Without daytime nap before pregnancy & sleep duration>7 h1013.6±2.72.3±2.21.3±1.2Daytime nap before pregnancy & sleep duration >7 h2143.8±2.72.4±2.31.4±1.2
ANCOVA was used to calculate the interaction of Sleep duration and daytime nap on FS-14 scores, *P<0.05
进一步对FS14总分、FS14躯体疲劳得分进行LSD简单效应分析发现,无午睡且夜眠≤7h-无午睡且夜眠>7h、无午睡且夜眠≤7h-午睡且夜眠≤7h、无午睡且夜眠≤7h-午睡且夜眠>7h、午睡且夜眠≤7h-无午睡且夜眠>7h的LSD值差异均具有统计学意义。见表4。
四、孕前午睡且目前夜眠时长≤7 h组孕妇夜眠时长与疲劳的关系
以年龄为协变量,实际夜眠时长分别与FS-14总分、FS-14躯体疲劳得分、FS-14脑力疲劳得分进行相关性分析,如图2所示,FS-14总分、FS-14躯体疲劳得分、FS-14脑力疲劳得分均与夜眠实际时长呈负相关。
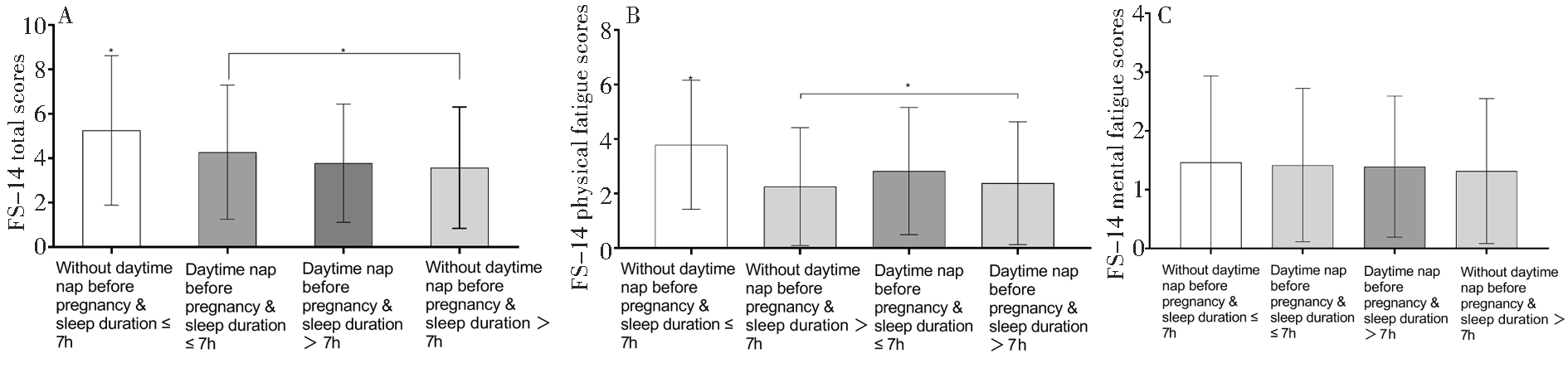
A:The differences of FS-14 fatigue total scores among four groups; B:The differences of FS-14 physical fatigue scores among four groups;C:The differences of FS-14 mental fatigue scores among four groups.*P<0.05
图1 各组间FS-14各项目得分比较
Figure 1 The effects of daytime nap before pregnancy and sleep duration on fatigue in the third trimester of pregnancy using general linear models
表3 孕前午睡与不同夜眠有效时长对孕晚期疲劳程度的影响
Table 3 The effects ofdaytime nap before pregnancy and sleep duration on fatigue in the third trimester of pregnancy

EffectsTotal fatigue scoresFPPhysical fatigue scoresFPMetal fatigue scoresFPDaytime nap (with or without)1.130.2892.410.1210.160.688Sleep duration≤ 7h / sleep duration > 7h14.440.000*18.120.000*0.780.378Daytime nap (with or without)×sleep duration(≤ 7h or > 7h)5.140.024*6.460.011*0.270.601
*P<0.05
表4 疲劳评分的简单效应分析
Table 4 The simple effect analysis of fatigue scores
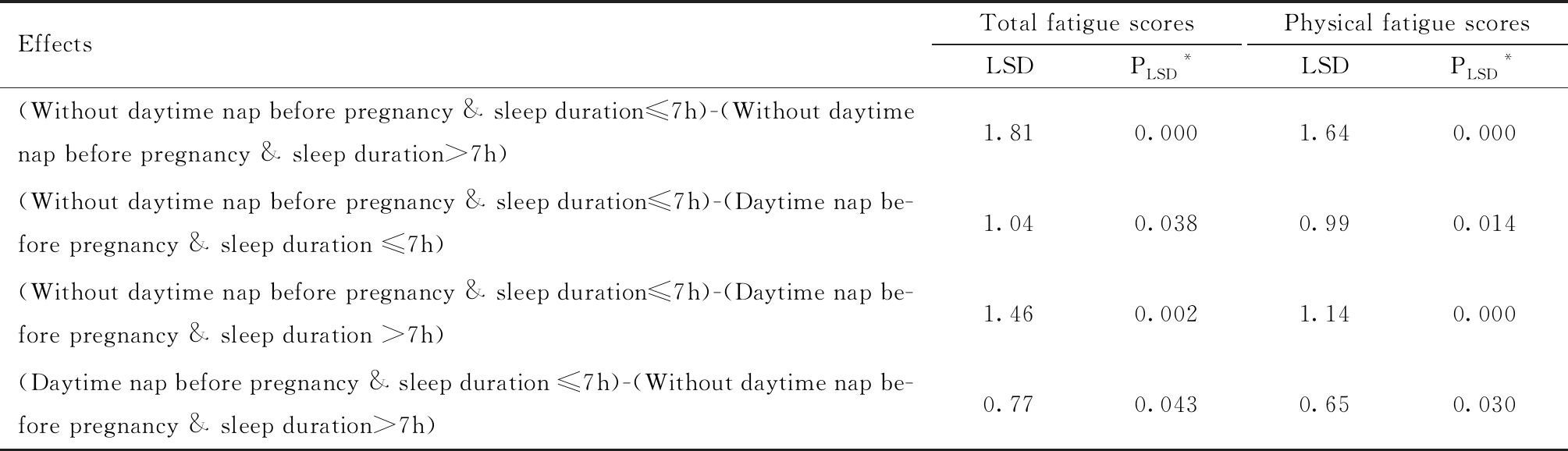
EffectsTotal fatigue scoresLSDPLSD*Physical fatigue scoresLSDPLSD*(Without daytime nap before pregnancy & sleep duration≤7h)-(Without daytime nap before pregnancy & sleep duration>7h)1.810.0001.640.000(Without daytime nap before pregnancy & sleep duration≤7h)-(Daytime nap be-fore pregnancy & sleep duration ≤7h)1.040.0380.990.014(Without daytime nap before pregnancy & sleep duration≤7h)-(Daytime nap be-fore pregnancy & sleep duration >7h)1.460.0021.140.000(Daytime nap before pregnancy & sleep duration ≤7h)-(Without daytime nap be-fore pregnancy & sleep duration>7h)0.770.0430.650.030
*P<0.05
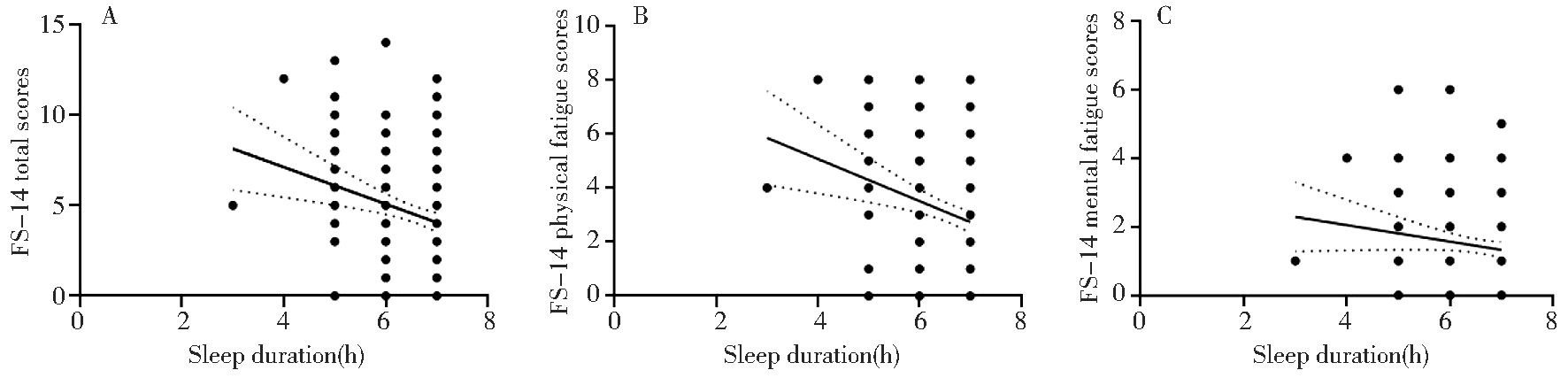
A:The correlation between FS-14 total score and sleep duration;B:The correlation between FS-14 physical fatigue score and sleep duration;C:The correlation between FS-14 mental fatigue score and sleep duration
图2 孕前午睡且目前夜眠时长≤7 h孕妇夜眠时长与疲劳的关系(以年龄为协变量)
Figure 2 The correlation between sleep duration and fatigue of pregnant women who took a nap before pregnancy and sleep duration in the third trimester ≤7 h
讨 论
本研究报道了孕前午睡与夜眠时长共同对孕晚期孕妇疲劳的影响。本研究主要发现是否午睡与夜眠时长的交互作用对FS-14总分、FS-14躯体疲劳得分存在影响,即孕前无午睡且夜眠≤7 h组孕妇FS-14总分、躯体疲劳得分均为最高分,表明该组孕妇最疲劳。究其原因,与该组孕妇每日睡眠总时长不足有关。Hall等[10]认为孕晚期妇女睡眠时长、睡眠质量与其疲劳症状存在负相关,Gay等[11]也提出疲劳与睡眠障碍呈正相关,且指出晚期孕妇疲劳得分与睡眠总时长有较高的相关度。本研究也发现,孕晚期妇女每日睡眠总时长越短其疲劳程度越为严重,通过对夜眠时长分别与FS-14各项得分行相关性分析,均呈负相关,表明夜眠时长>7 h对缓解躯体疲劳具有积极作用。
研究发现,午睡可以减少主观疲劳并改善身体机能[12],并且午睡对身体机能的有益影响,与前一晚的睡眠无关[13]。根据现有研究结论,长期午睡对身体机能存在诸多方面的改善作用,如(1)改善神经内分泌功能、促进免疫系统功能的恢复[14],其主要机制与午睡影响IL-6及儿茶酚胺分泌有关[15];(2)午睡后皮质醇水平下降可产生缓解疲劳的效果[16];(3)国外一项关于健康成人午睡与冠心病死亡率研究发现,在控制混杂因素后,健康人群午睡与冠心病死亡率呈负相关[17];(4)午睡对恢复警觉性、改善记忆力、改善情绪状态均有积极作用。本研究记录被试者孕前午睡情况,尽管未直接调查其与午睡相关的积累效应,但通过数据分析,可以看出午睡组孕妇疲劳程度在各组中处于适中水平,表明午睡对缓解疲劳具有积极作用。
脑力疲劳最早由Prince[18]于1960年提出,一般认为它是与躯体疲劳相对立的用以描述疲劳的另外一个子类,主要涉及注意力、思维能力、语言表达能力、记忆力、兴趣爱好等方面。基于对医护人员[19]、建筑工人脑力疲劳及躯体疲劳的研究[20],躯体疲劳、脑力疲劳之间存在何种相关性,目前仍缺少统一结论。本研究发现,妊娠晚期妇女的FS-14脑力疲劳得分差异无统计学意义,且未出现躯体疲劳得分与脑力疲劳得分同步增高的现象,表明脑力疲劳受夜眠时长和是否孕前午睡的影响可能较小。本研究还发现,教育程度存在组间差异,考虑与现阶段育龄期女性受教育程度偏向高学历层次有关,这种构成比例与国内第七次人口普查教育相关数据表现一致。因一般资料问卷、FS-14评分量表内容均易于理解,故本研究中,教育程度的差异不影响问卷及量表调查。
本研究局限性在于,因时间距离较久未能问询孕前午睡具体时长,这可能有助于发现最佳午睡时间范围。
综上所述,孕前无午睡且目前夜眠时长小于7 h对孕妇目前的疲劳程度影响最大,其中主要体现为躯体疲劳。为了优生优育、计划内怀孕妇女应保持孕前午睡的习惯且持久的夜眠最好大于7 h;对于孕前没有午睡习惯的孕妇,为了降低疲劳应保持夜眠时长>7 h。本研究拟后期追踪随访该批被试,并招募孕后午睡的被试,进一步比较午睡对孕晚期妇女疲劳的影响。
1 白丽娟,吴建杰,张玉涛,等.妊娠期睡眠生理及睡眠障碍的研究进展.中国全科医学,2020,23:125-133.
2 Hirshkowitz M,Whiton K,Albert SM,et al.National sleep foundation′s updated sleep duration recommendations:final report.Sleep Health,2015,1:233-243.
3 杜敏,刘珏.孕期睡眠障碍的流行病学研究进展.中国生育健康杂志,2020,31:81-83.
4 Xu X,Liu D,Zhang Z,et al.Sleep duration and quality in pregnant women:a cross-sectional survey in china.Int j environ res public health,2017,14:817.
5 Rodriguez A,Bohlin G,Lindmark G.Symptoms across pregnancy in relation to psychosocial and biomedical factors.ActaObstet Gynecol Scand,2001,80:213-223.
6 Williams MA,Miller RS,Qiu C,et al.Associations of early pregnancy sleep duration with trimester-specific blood pressures and hypertensive disorders in pregnancy.Sleep.2010,33:1363-1371.
7 Tsai SY,Lin JW,Kuo LT,et al.Daily sleep and fatigue characteristics in nulliparous women during the third trimester of pregnancy.Sleep,2012,35:257-262.
8 Zheng X,Zhang L,Shen L,et al.Maternal habitual midday napping duration and frequency are associated with high birthweight.Sci rep,2017 ,7:10564.
9 Chalder T,Berelowitz G,Pawlikowska T,et al.Development of a fatigue scale.J Psychosom Res,1993,37:147-153.
10 Hall WA,Hauck YL,Carty EM,et al.Childbirth fear,anxiety,fatigue,and sleep deprivation in pregnant women.J Obstet Gynecol Neonatal Nurs,2009 ,38:567-576.
11 Gay CL,Lee KA,Lee SY.Sleep patterns and fatigue in new mothers and fathers.Biol ResNurs,2004 ,5:311-318.
12 Hsouna H,Boukhris O,Abdessalem R,et al.Effect of different nap opportunity durations on short-term maximal performance,attention,feelings,muscle soreness,fatigue,stress and sleep.Physiol Behav,2019,211:112673.
13 Boukhris O,Trabelsi K,Ammar A,et al.A 90 min daytime nap opportunity is better than 40 min for cognitive and physical performance.Int J Environ Res Public Health,2020,17:4650.
14 Faraut B,Andrillon T,Vecchierini MF,et al.Napping:a public health issue.From epidemiological to laboratory studies.Sleep Med Rev,2017,35:85-100.
15 Faraut B,Nakib S,Drogou C,et al.Napping reverses the salivary interleukin-6 and urinary norepinephrine changes induced by sleep restriction.J Clin Endocrinol Metab,2015 ,100:416-426.
16 Faraut B,Boudjeltia KZ,Dyzma M,et al.Benefits of napping and an extended duration of recovery sleep on alertness and immune cells after acute sleep restriction.Brain Behav Immun,2011,25:16-24.
17 Naska A,Oikonomou E,Trichopoulou A,et al.Siesta in healthy adults and coronary mortality in the general population.Arch Intern Med,2007,167:296-301.
18 Prince R.The "brain fag" syndrome innigerian students.J Ment Sci,1960 ,106:559-570.
19 宋爱芹,李印龙,翟景花,等.FAI与FS-14对济宁市女性医护人员疲劳评定的关联性分析.济宁医学院学报,2010,33:140-142.
20 Xing X,Zhong B,Luo H,et al.Effects of physical fatigue on the induction of mental fatigue of construction workers:a pilot study based on a neurophysiological approach.Automat Constr,2020,120:1-11.