剖宫产率的高低一直备受关注,成为重要的公共卫生问题[1]。随着全面二孩政策的开放,经产妇人群增多,瘢痕子宫产妇再次妊娠分娩所产生的健康安全问题引起医界重视,因此有效降低剖宫产率再度成为社会共识[2]。WHO建议使用Robson分类系统[3]对产妇人群特征进行分层,可减少混杂因素的干扰,本文将初产妇和经产妇分别应用Robson分类法分组,更能清晰地体现不同产妇特点,为全面二孩政策下初产妇和经产妇剖宫产率的控制提供策略方案,降低剖宫产率,提高母婴安全。
对象与方法
一、研究对象
以2016年1月1日—2019年12月31日在大连某妇幼保健院分娩的全部孕妇为研究对象,去除28周以下的活产、死产、死胎病例,共纳入61 691例。其中初产妇45 520例,经产妇16 171例。
二、研究方法
1.资料清理:利用产妇病案首页的机构化电子信息,对采集数据的人员进行培训,详细阅读病例后根据Robson分类法的五个重要产科特征,将产妇分为10组,采集的数据和所做的分类均经重复校对,确保分组的准确性。
2.Robson分类法[3]:该分类法将所有产妇分为10类,10组人群既不重复又能包含全部人群。根据产次、临产方式、孕周、胎位、胎儿数量迅速将产妇归类到相应组别。详细分组见表1。本文中各组产妇构成比,是各组产妇例数占总产妇例数的百分比;剖宫产构成比是各组中剖宫产例数与总剖宫产例数的百分比;组内剖宫产率是各组剖宫产例数占同组产妇例数的比例;总剖宫产率是各组剖宫产例数占总产妇例数的比例。
表1 不同Robson分类总产妇特征和剖宫产情况
Table 1 Cesarean delivery rate according to Robson classification
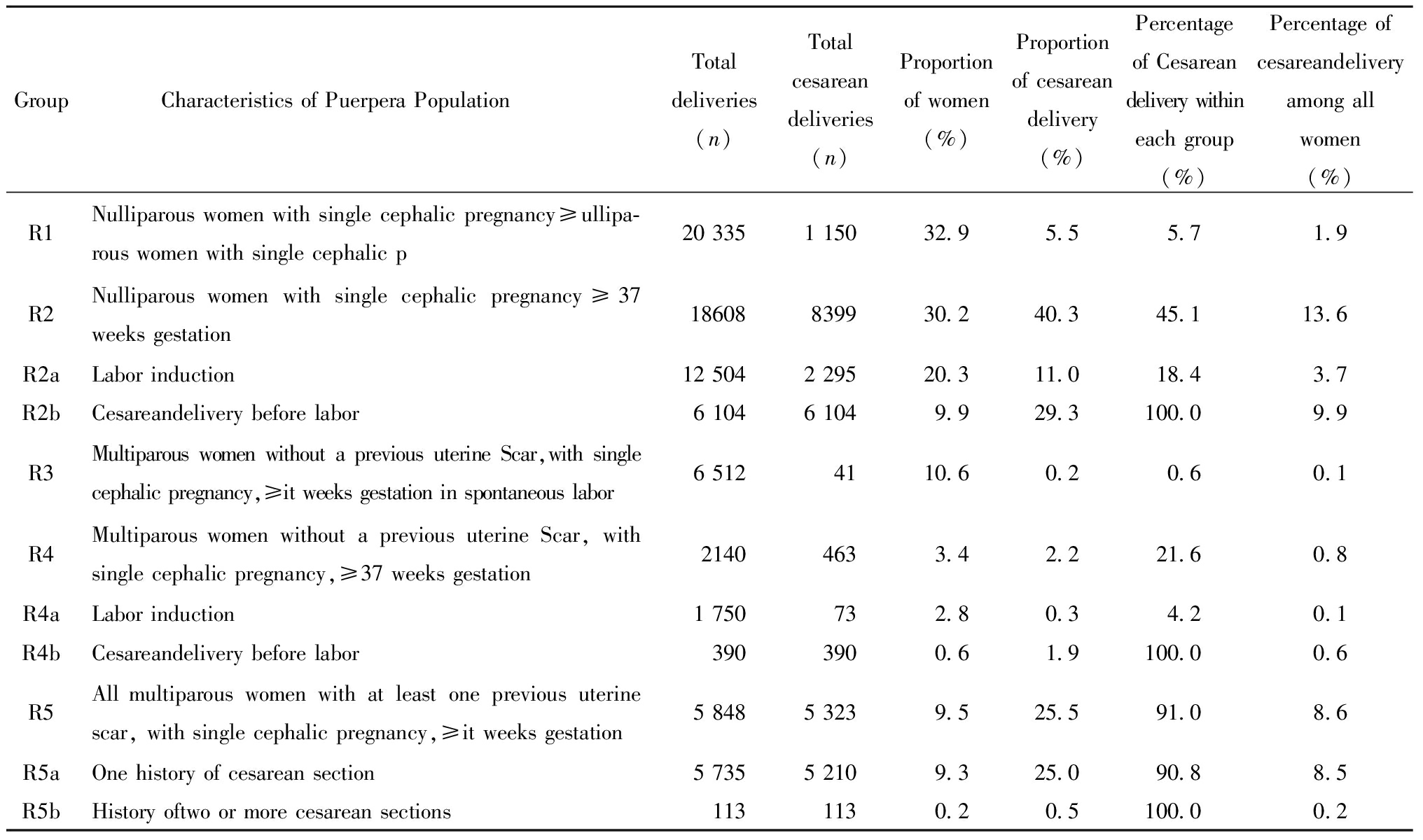
Group Characteristics of Puerpera PopulationTotal deliveries(n)Total cesareandeliveries(n)Proportion of women (%)Proportion of cesarean delivery(%)Percentage of Cesareandelivery withineach group(%)Percentage of cesareandelivery among all women (%)R1Nulliparous women with single cephalic pregnancy≥ullipa-rous women with single cephalic p20 3351 15032.95.55.71.9R2Nulliparous women with single cephalic pregnancy≥37 weeks gestation18608839930.240.345.1 13.6 R2aLabor induction12 5042 29520.311.018.43.7R2bCesareandelivery before labor6 1046 1049.929.3100.09.9R3Multiparous women without a previous uterine Scar,with single cephalic pregnancy,≥it weeks gestation in spontaneous labor6 5124110.60.20.60.1R4Multiparous women without a previous uterine Scar, with single cephalic pregnancy,≥37 weeks gestation21404633.42.2 21.60.8R4aLabor induction1 750732.80.3 4.20.1R4bCesareandelivery before labor3903900.61.9100.00.6R5All multiparous women with at least one previous uterine scar, with single cephalic pregnancy,≥it weeks gestation5 8485 3239.525.591.08.6R5aOne history of cesarean section5 7355 2109.325.090.8 8.5R5bHistory oftwo or more cesarean sections1131130.20.5100.00.2
表1(续)

Group Characteristics of Puerpera PopulationTotal deliveries(n)Total cesareandeliveries(n)Proportion of women (%)Proportion of cesarean delivery(%)Percentage of Cesareandelivery withineach group(%)Percentage of cesareandelivery among all women (%)R6All nulliparous women with a single breech pregnancy2 4172 3703.911.498.13.8R7All multiparous women with a single breech Pregnancy, in-cluding women with previous uterine scars4944760.82.396.40.8R8All women with multiple pregnancies, including women with previous uterine scars1 4081 1292.35.480.21.8R9All women with a single pregnancy with a transverse or ob-lique lie, including women with previous uterine scars67660.10.398.50.1R10All women with a single cephalic pregnancy<37 weeks ges-tation, including women with previous scars3 8621 4326.36.937.12.3Total61 69120 84910010033.833.8
3.统计学分析:运用SPSS 23.0软件对数据进行处理和统计分析,计数资料用百分率(%)表示,产妇构成比、剖宫产构成比及组内剖宫产率分布用趋势性χ2检验,P<0.05 为差异有统计学意义。
结 果
一、不同Robson分类总产妇特征和剖宫产率情况
由表1可知,产妇共有61 691例,人群构成比占前三位的是R1(初产妇单胎头位,足月,自然临产)、R2a(初产妇单胎头位,足月、引产临产)和R3组(经产妇单胎头位,足月,自然临产),剖宫产构成比前三位的是R2b组(初产妇单胎头位,足月,临产前剖宫产)、R5a组(有1次剖宫产史的经产妇)和R6组(所有初产妇单胎臀位)。四年剖宫产共计20 849例,总剖宫产率为33.8%。详见表1。
二、不同Robson分类初产妇人群及剖宫产率变化趋势
初产妇45 520例,占全部产妇的73.8%,初产妇剖宫产13 983例,2016—2019年初产妇总剖宫产率为30.7%(13 983/45 520),初产妇剖宫产率呈上升趋势(P<0.05)。Robson分类法下,初产妇人群构成比前三位依次是R1组(初产妇单胎头位,足月,自然临产)、R2a组(初产妇单胎头位,足月,引产临产)、R2b组(初产妇单胎头位,足月,临产前剖宫产)。R2a组(初产妇单胎头位,足月,引产临产)、R6组(所有初产妇单胎臀位)和R9组(单胎横位或斜位初产妇)四年间构成比呈上升趋势,R1组(初产妇单胎头位,足月,自然临产)和R10组(早产初产妇)呈下降趋势(P均<0.05);剖宫产构成比前3位依次是R2a组(初产妇单胎头位,足月,引产临产)、R2b组(初产妇单胎头位,足月,临产前剖宫产)和R6组(所有初产妇单胎臀位),R2a组(初产妇单胎头位,足月,引产临产)和R9组(单胎横位或斜位的初产妇)四年间剖宫产构成比呈上升趋势,R10组(早产的初产妇)呈下降趋势(P均<0.05);R1组(初产妇单胎头位,足月,自然临产)和R8组(双胎妊娠初产妇)组内剖宫产率呈上升趋势(P均<0.05)。详见表2。
表2 不同Robson分类初产妇人群特征和剖宫产率情况分析[例(%)]
Table 2 Cesarean delivery rate according to Robson classification among primiparous women, 2016-2019[n(%)]
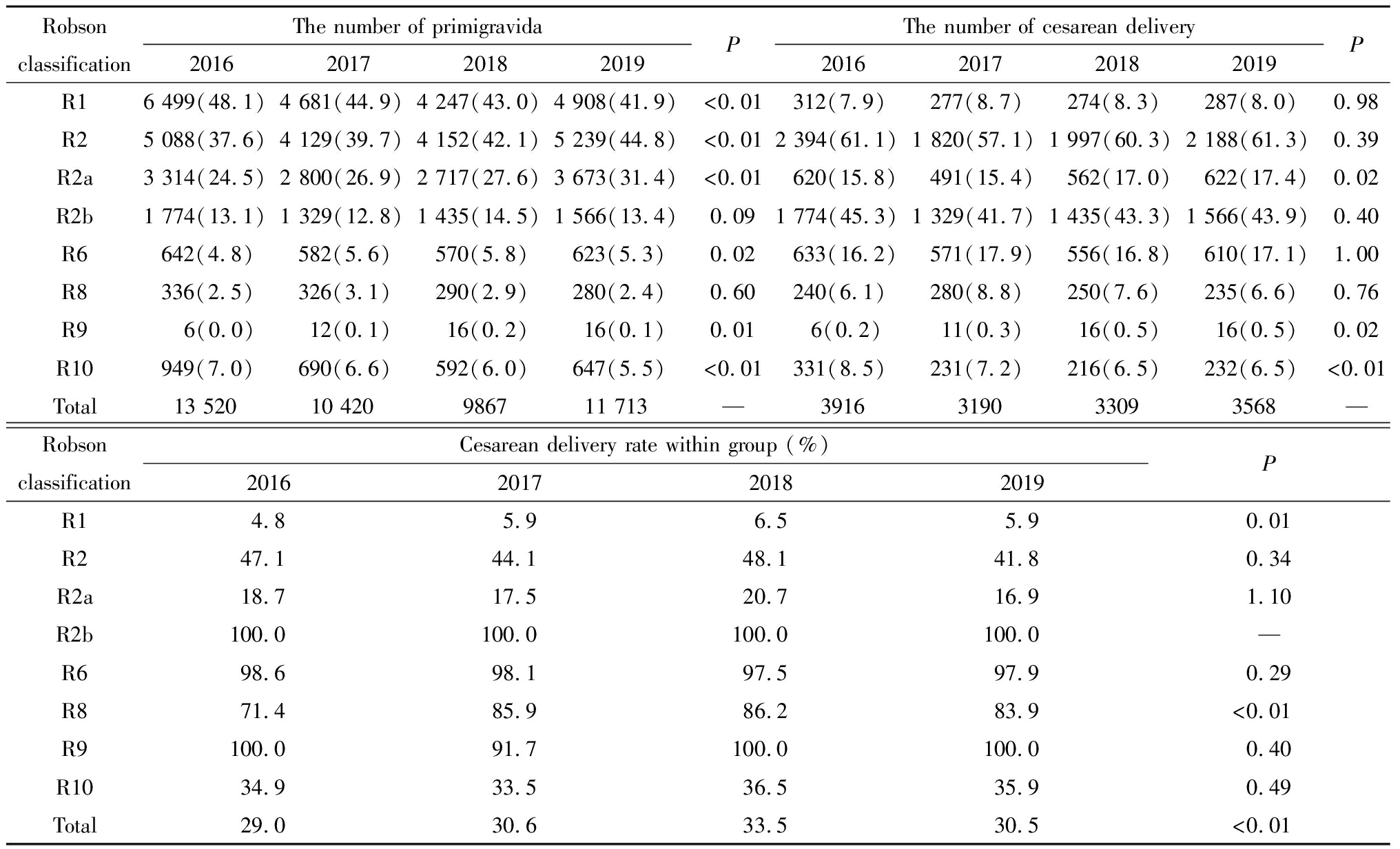
Robson classificationThe number of primigravida2016201720182019PThe number of cesarean delivery2016201720182019PR16 499(48.1)4 681(44.9)4 247(43.0)4 908(41.9)<0.01312(7.9)277(8.7)274(8.3)287(8.0)0.98R25 088(37.6)4 129(39.7)4 152(42.1)5 239(44.8)<0.012 394(61.1)1 820(57.1)1 997(60.3)2 188(61.3)0.39R2a3 314(24.5)2 800(26.9)2 717(27.6)3 673(31.4)<0.01620(15.8)491(15.4)562(17.0)622(17.4)0.02R2b1 774(13.1)1 329(12.8)1 435(14.5)1 566(13.4)0.091 774(45.3)1 329(41.7)1 435(43.3)1 566(43.9)0.40R6642(4.8)582(5.6)570(5.8)623(5.3)0.02633(16.2)571(17.9)556(16.8)610(17.1)1.00R8336(2.5)326(3.1)290(2.9)280(2.4)0.60240(6.1)280(8.8)250(7.6)235(6.6)0.76R96(0.0)12(0.1)16(0.2)16(0.1)0.016(0.2)11(0.3)16(0.5)16(0.5)0.02R10949(7.0)690(6.6)592(6.0)647(5.5)<0.01331(8.5)231(7.2)216(6.5)232(6.5)<0.01Total 13 520 10 420 9867 11 713— 3916 3190 3309 3568—Robson classificationCesarean delivery rate within group (%)2016201720182019PR14.85.96.55.90.01R247.144.148.141.80.34R2a18.717.520.716.91.10R2b100.0100.0100.0100.0—R698.698.197.597.90.29R871.485.986.283.9<0.01R9100.091.7100.0100.00.40R1034.933.536.535.90.49Total29.030.633.530.5<0.01
三、不同Robson分类经产妇人群及剖宫产率变化趋势
61 691例产妇中,经产妇16 171例,占26.2%,剖宫产例数6 866例,2016—2019年经产妇总剖宫产率为42.5%(6 866/16 171),经产妇剖宫产率呈下降趋势(P<0.05)。Robson分类法下,经产妇人群构成比前三位依次是 R3组(经产妇单胎头位,足月,自然临产)、R5a组(有1次剖宫产史的经产妇)、R4a组(经产妇单胎头位,足月、引产临产)。R4a组(经产妇单胎头位,足月、引产临产)构成比四年间呈上升趋势,R4b组(经产妇单胎头位,足月,临产前剖宫产)、R5a组(有1次剖宫产史的经产妇)、R7组(所有经产妇、单胎臀位)和R10组(早产的经产妇)呈下降趋势(P均<0.05);剖宫产构成比前3位依次是R5a组(有1次剖宫产史的经产妇)、R7组(所有经产妇、单胎臀位)和R10组(早产的经产妇)。R5a组(有1次剖宫产史的经产妇)剖宫产构成比呈上升趋势,R10组(早产的经产妇)呈下降趋势(P均<0.05);组内剖宫产率中R8组(双胎妊娠经产妇)呈上升趋势,R4组(经产妇无剖宫产史,单胎头位,足月)呈下降趋势(P均<0.05)。详见表3。
表3 不同Robson分类经产妇人群特征和剖宫产率情况分析[例(%)]
Table 3 Cesarean delivery rate according to Robson classification among multiparous women, 2016-2019[n(%)]
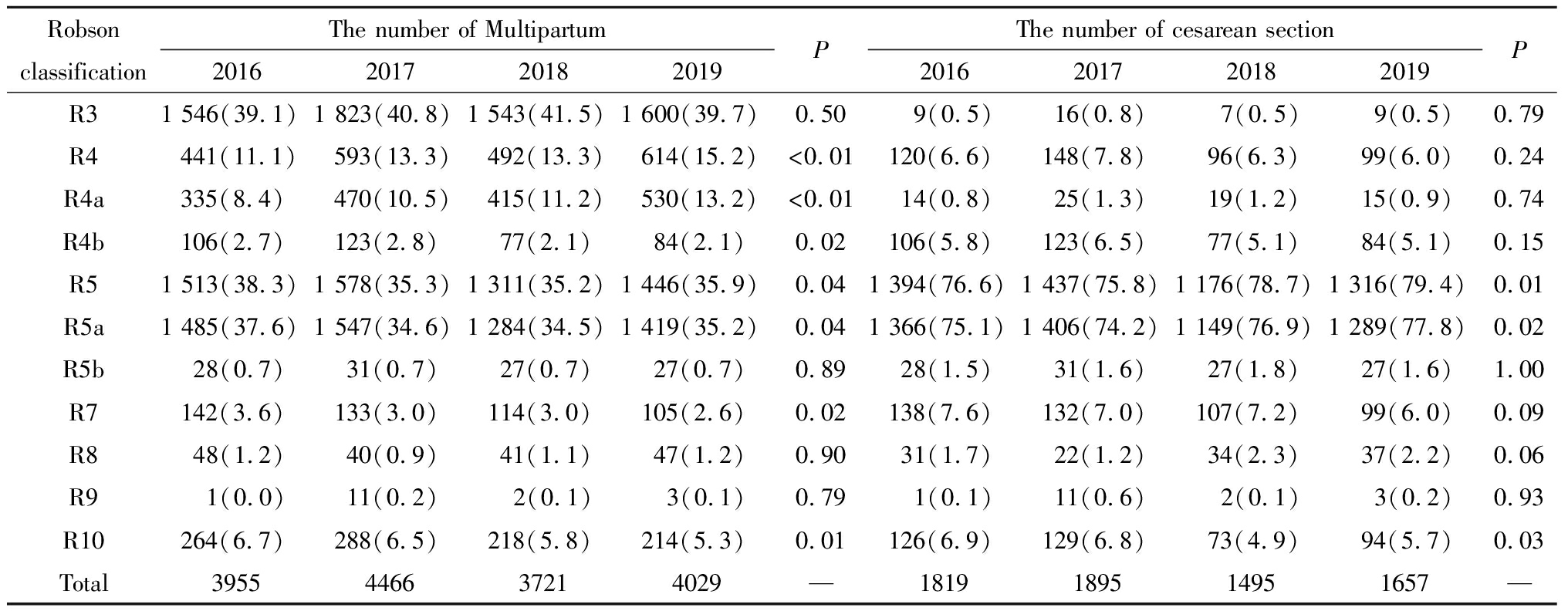
Robson classificationThe number of Multipartum2016201720182019PThe number of cesarean section2016201720182019PR31 546(39.1)1 823(40.8)1 543(41.5)1 600(39.7)0.509(0.5)16(0.8)7(0.5)9(0.5)0.79R4441(11.1)593(13.3)492(13.3)614(15.2)<0.01120(6.6)148(7.8)96(6.3)99(6.0)0.24R4a335(8.4)470(10.5)415(11.2)530(13.2)<0.0114(0.8)25(1.3)19(1.2)15(0.9)0.74R4b106(2.7)123(2.8)77(2.1)84(2.1)0.02106(5.8)123(6.5)77(5.1)84(5.1)0.15R51 513(38.3)1 578(35.3)1 311(35.2)1 446(35.9)0.041 394(76.6)1 437(75.8)1 176(78.7)1 316(79.4)0.01R5a1 485(37.6)1 547(34.6)1 284(34.5)1 419(35.2)0.041 366(75.1)1 406(74.2)1 149(76.9)1 289(77.8)0.02R5b28(0.7)31(0.7)27(0.7)27(0.7)0.8928(1.5)31(1.6)27(1.8)27(1.6)1.00R7142(3.6)133(3.0)114(3.0)105(2.6)0.02138(7.6)132(7.0)107(7.2)99(6.0)0.09R848(1.2)40(0.9)41(1.1)47(1.2)0.9031(1.7)22(1.2)34(2.3)37(2.2)0.06R91(0.0)11(0.2)2(0.1)3(0.1)0.791(0.1)11(0.6)2(0.1)3(0.2)0.93R10264(6.7)288(6.5)218(5.8)214(5.3)0.01126(6.9)129(6.8)73(4.9)94(5.7)0.03Total 3955 4466 3721 4029— 1819 1895 1495 1657 —
表3(续)
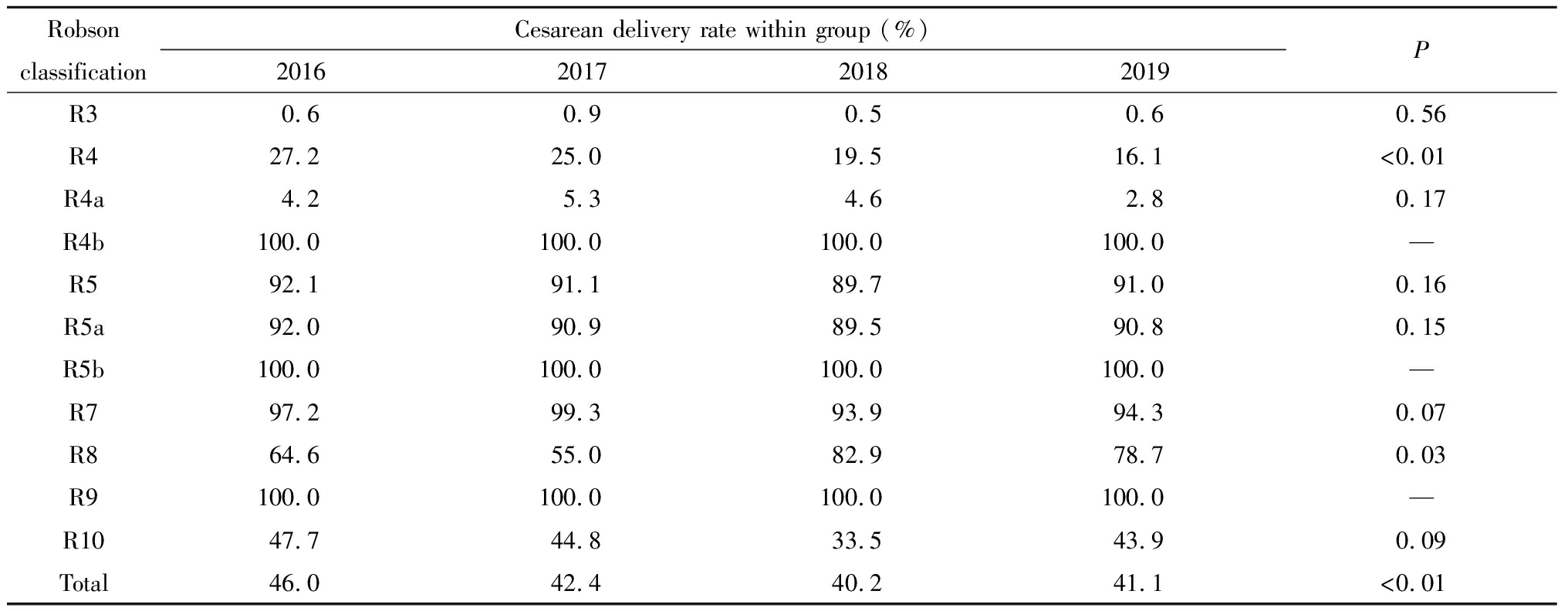
Robson classificationCesarean delivery rate within group (%)2016201720182019PR30.60.90.50.60.56R427.225.019.516.1<0.01R4a4.25.34.62.80.17R4b100.0100.0100.0100.0—R592.191.189.791.00.16R5a92.090.989.590.80.15R5b100.0100.0100.0100.0—R797.299.393.994.30.07R864.655.082.978.70.03R9100.0100.0100.0100.0—R1047.744.833.543.90.09Total46.042.440.241.1<0.01
讨 论
本研究分析了“全面二孩”政策后的四年间该院剖宫产率控制的基本情况,总剖宫产率为33.8%,低于世界卫生组织在2015年关于中国剖宫产率(47.6%)的报道[4],同时低于上海与广州的报道[5-6],但高于拉丁美洲(26.4%),与WHO推荐的剖宫产率5%~15%仍相差甚远[7]。本研究发现对总剖宫产率影响最大的组群是R2b(初产妇单胎头位,足月,临产前剖宫产)、R5a(有1次剖宫产史的经产妇)、R6组(所有初产妇单胎臀位),与王佳等人研究结果相似[8]。蒋红清等[9]对北京市地区产妇剖宫产率的研究提示中国继“全面二孩”政策后剖宫产率仍维持在较高水平,并建议严格控制经产妇的无指征剖宫产。本研究通过Robson分类法全面地呈现出初产妇和经产妇人群的构成比、剖宫产构成比及剖宫产率变化,对各组进行分类研究。
一、全面二孩政策下初产妇剖宫率的控制
2016年“全面二孩”政策放开后,本院初产妇剖宫产率呈逐年上升趋势,提示初产妇仍是控制剖宫产率的重点人群,与2014年美国妇产科医师协会和母胎医学会就联合呼吁出台安全降低初次剖宫产率的政策初衷相吻合[10]。初产妇规模较大的组群是R1组(初产妇单胎头位,足月,自然临产)、R2a组(初产妇单胎头位,足月,引产临产)、R2b组(初产妇单胎头位,足月,临产前剖宫产),对剖产率影响较大的组群则是R2a组(初产妇单胎头位,足月,引产临产)、R2b组(初产妇单胎头位,足月,临产前剖宫产)、R6组(所有初产妇单胎臀位)。
R1组(初产妇单胎头位,足月,自然临产)是最大的初产妇组群,组内剖宫产率不高但呈逐年上升趋势,对总剖宫产率影响不大,但在临床实践中仍需避免产妇临产后发生中转剖宫产的可能[11]。
R2a组(初产妇单胎头位,足月,引产临产)无论是产妇构成比还是剖宫产构成比均占初产妇前三位,位居总产妇人群构成比位第二,且趋势逐年上升,对初产妇剖宫产率的影响至关重要。R2b组(初产妇单胎头位,足月,临产前剖宫产)虽然产妇构成比、剖宫产构成比没有逐年上升,但仍稳居前三位。因此,降低R2组(初产妇单胎头位,足月)人群的剖宫产率是降低初产妇人群的剖宫产率的关键。R2组(初产妇单胎头位,足月)人群剖宫产率控制不当会直接导致R5a(有1次剖宫产史的经产妇)人群增大,对控制总剖宫产率带来不利因素。控制R2a组(初产妇单胎头位,足月,引产临产)人群剖宫产率,医生应按照产科规范和指南,掌握好引产指征,配合使用分娩镇痛,有效降低中转剖宫产率等措施[12]。R2b组(初产妇单胎头位,足月,临产前剖宫产)人群多因高龄初产、巨大儿或者一些社会因素而选择剖宫产,因此针对这部分人群应该提倡孕产期保健,门诊产检时医生应注重营养指导及体重增长管理等优生优育策略,减少巨大儿的发生。Ji[13]等剖宫产高危因素调查显示,医生的建议和孕妇对阴道分娩的信心也是控制剖宫产率的重要因素,因此R2b组(初产妇单胎头位,足月,临产前剖宫产)中的无指征剖宫产和放宽指征剖宫产人群,医生应积极鼓励,对产道条件和胎儿大小进行综合评估,提供试产机会。
R6组(所有初产妇单胎臀位)产妇人群规模逐年上升,对初产妇剖宫产率贡献占第3位,该组剖宫产指征为臀位,组内剖宫产率达98%,针对该组产妇,可以施行外倒转术(external cephalic version,ECV)。有研究表明:足月及近足月妊娠行ECV可以减少非头位胎儿的剖宫产率[14]。随着中国“全面二孩”政策的实施,孕妇自然分娩的意愿增加,建议经过充分评估,选择合适的孕妇,在具备行紧急剖宫产术条件的医疗机构进行ECV,以保障母儿安全[15]。本院从2019年开展了外倒转术,今后的研究可进一步分析其成果。
R8组(双胎妊娠初产妇)虽然组内剖宫产率呈上升趋势,但由于产妇人数所占比例对总剖宫产率影响甚小,且双胎妊娠本身对医生和孕妇都具挑战性,故不作为主要降低剖宫产的人群。同理R9组(单胎横位或斜位初产妇)、R10组(早产初产妇)亦不作为降低初产妇人群剖宫产率的重点人群。
二、全面二孩政策下经产妇剖宫率的控制
四年间,经产妇总剖宫产率占42.5%,呈下降趋势,但仍高于总剖宫产率水平。对剖宫产率影响较大的经产妇组群是R5a组(有一次剖宫产的经产妇)、R7组(所有经产妇、单胎臀位、包括有剖宫产史的产妇)、R10组(所有单胎头位<37周的经产妇)。
R5a组(有一次剖宫产的经产妇)是经产妇人群中第二大组群,剖宫产构成比逐年上升,对经产妇剖宫产率和总剖宫产率影响较大。在R5a组(有一次剖宫产的经产妇)人群中推行剖宫产后经阴分娩(VBAC)[16]有望降低该组剖宫产率,降低该组人群对总剖宫产率的影响,国外多项VBAC安全性和可行性的研究发现VBAC成功率可达54%~75%[17-18],近年来国内的报道亦显示VBAC成功率逐年上升[19],因此积极宣教和充分告知对VBAC的实施至关重要。对具备急救条件及技术水平的医院可尝试推行剖宫产后经阴道分娩,对不具备以上条件的基层医院需慎重选择VBAC,可从降低初产妇人群的剖宫产率上入手,使再生育时瘢痕子宫的孕产妇,即R5a组(有一次剖宫产的经产妇)人群规模缩小,降低其对总剖宫产率的影响。
R7组中单胎臀位的经产妇,虽然近几年人数略有下降,但是剖宫产构成比占经产妇的第二位。王晓怡[20]对500例臀位孕妇施行外倒转术的研究表明,经产妇行外倒转术的成功率是初产妇的3.74倍,产次是外倒转成功的主要影响因素,再次妊娠的经产妇人群可以通过外倒转术降低剖宫产率。
R10组中早产的经产妇,对经产妇剖宫产率影响位居第三。该组经产妇构成比虽逐年下降,但组内剖宫产率逐年上升,究其原因可能是二孩政策实施后,经产妇年龄普遍增大,该院最大产妇年龄为50岁,妊娠期糖尿病、高血压、胎盘早剥等疾病的发生率增大,且其中不乏瘢痕妊娠者,故不得不进行剖宫产[21]。建议在全面二孩政策后医院应加强对经产妇的管理,特别是对有晚期流产或习惯性早产史的经产妇及高龄人群进行全程围产期监督与管理[22]。
综上所述,在全面二孩政策下,对初产妇剖宫产率的控制应重点关注单胎头位足月以及所有单胎臀位的初产妇人群,对经产妇剖宫产率的控制应重点关注有1次剖宫产史、所有单胎臀位以及早产的经产妇人群。未来控制总剖宫产率的重点仍需放在初产妇人群上,临床医生需对初产妇和经产妇制定个性化诊疗体系,最终降低剖宫产率改善母婴预后。
1 Vogel JP,Betrán AP,Vindevoghel N,et al.Use of the Robson classification to assess caesarean delivery trends in 21 countries:a secondary analysis of two WHO multicountry surveys.Lancet Glob Health,2015,3:e260-270.
2 Li HT,Luo S,Trasande L,et a1.Geographic variations and temporal trends in cesarean delivery rates in China,2008-2014.JAMA,2017,317:69-76.
3 Robson M,MurphyM,BymeF.Quality assurance:the 10-group classification system(Robson classification),induction of labor,and cesarean delivery.Int J Gynaecol Obstet,2015,131 Suppl 1:s23-27.
4 Vogel JP,Betrfin AP,Vindevoghel N,et a1.Use of the Robson classification to assess caesarean delivery trends in 21 countries:a secondary analysis of two WHO multicountry surveys.Lancet Glob Health,2015,3:e260-270.
5 花静,刘铭,严晓玲,等.以Robson十分类法为基础的剖宫产率关联因素和预测效度.中华围产医学杂志,2017,20:104-109.
6 邓松清,陈海天,王冬昱,等.二孩政策前后剖宫产率及剖宫产指征变化.中华围产医学杂志,2017,20:47-50.
7 Barcaite E,Kemekliene G,Railaite DR,et al.Cesarean delivery rates in Lithuania using Robson ten group classification system.Medicina(Kaunas),2015,51:280-285.
8 王佳,黄沁,蒋琳,等.以Robson十分类法研究“二孩政策”对剖宫产率的影响.中华围产医学杂志,2018,10:694-696.
9 蒋红清,陈寒,杨静.Robson十分类系统在剖宫产率分析中的应用研究.中国妇幼保健,2016,31:4349-4353.
10 Caughey AB,Cahill AG,Guise JM,et al.Safe prevention of the primary cesarean delivery.Am J Obstet Gynecol,2014,210:179-193.
11 孙雯,王晓怡,余琳,等.基于Robson分类系统分析不同类型的阴道试产失败中转剖宫产的构成及母儿结局.中华妇产科杂志,2019,5:512-515.
12 郑嫒媛,邹丽颖,范玲.新产程标准实施后产程中剖宫产指征的变化及母儿预后分析.中华妇产科杂志,2016,51:245-249.
13 Ji HL,Jiang H,Yang LM,et al.Factors contributing to the rapid rise of caesarean section:a prospective study of primiparous Chinese women in Shanghai.BMJ Open,2015,5:e008994.
14 Hofmeyr GJ,Kulier R,West HM.External cephalic version for breech presentation at term.Cochrane Database Syst Rev,2015:CD000083.
15 龙俊青,韦红卫,夏红卫,等.足月及近足月外倒转术的成功率及其影响因素分析.中华妇产科杂志,2019,54:516-521.
16 American College of Obstetricians and Gynecologists.ACOG Practice bulletin no.115:Vaginal birth after previous cesarean delivery.Obstet Gynecol,2010,116:450-463.
17 Ryan GA,Nicholson SM,Morrison JJ.Vaginal birth after caesarean section:Current status and where to from here?.Eur J Obstet Gynecol Reprod Biol,2018,224:52-57.
18 Knight HE,Gurol-UrganciI,van der Meμlen JH,et al.Vaginal birth after caesarean section:a cohort study investigating factors associated with its uptake and success.BJOG,2014,121:183-192.
19 韩肖燕,杨桦.剖宫产术后再次妊娠阴道分娩的临床效果及安全性评价.中华妇产科杂志 ,2019,54:411-414.
20 王晓怡,柯彩萍.再谈臀位外倒转术.中华产科急救电子杂志,2018,7:148-152.
21 Ben-David A,Glasser S,Schiff E,et al.Pregnancy and birth out-comes among primiparae at very advanced maternal age:at what price?.Maternal Child Health J,2015,9:94-103.
22 McIntosh J,FehovichH,BerghellaV,et al.The role of routine cervical length screening in selected high-and low-risk women for preterm birth prevention.Am J Obstet Gynecol,2016,215:B2-B7.