个体的生长发育是一个连续的过程,0~3岁婴幼儿体格发育是儿童乃至成人期体格发育的基础[1-4],婴幼儿期体格发育过速或过缓均不利于个体的生长发育,甚至与儿童期肥胖、青春发动时相提前、2型糖尿病、心血管疾病、代谢综合征等疾病发病风险相关[1-8]。婴幼儿生长发育受到基因和环境的共同影响,具有一定的异质性,其中环境因素包括宫内生长受限、喂养情况、自身疾病状态等近端因素和社会经济等远端因素[9-11]。探讨婴幼儿期体格发育趋势,筛选出对体格发育产生影响的可控因素,对个体生长发育及健康状态具有重要意义。大数据概念的提出使得基于群组轨迹模型(group-based trajectory model,GBTM)越来越受到学者的关注,此模型可将个体的纵向重复测量数据科学的分配至有限个轨迹组别中,有利于识别群体中可能存在的增长轨迹亚组[12-13]。体质量指数Z分值(BMI-for-age z-score,Z-BMI)是评价婴幼儿期体格状态简约且有意义的指标,目前已被研究者广泛纳入GBTM分析,用于评价个体的体格发育轨迹,但现有研究多在发达国家进行,并且涵盖的年龄范围不同[14-23],缺乏针对中国3岁以内婴幼儿的研究[24-28]。此外,现有探讨婴幼儿Z-BMI轨迹影响因素的研究有限且结果尚未达成共识[23-25]。因此,本研究以中国疾病预防控制中心妇幼保健中心的母婴健康动态监测队列为基础,以Z-BMI为体格发育评价指标,采用GBTM分析0~3岁婴幼儿的体格发育轨迹,并采用无序多分类Logistic回归模型分析不同体格发育轨迹的潜在影响因素,为促进婴幼儿健康发育提供参考。
对象与方法
一、研究对象
研究对象来自中国疾病预防控制中心妇幼保健中心的母婴健康动态监测队列。采用前瞻性队列研究设计,基于方便抽样方法,于2015年9月—2019年6月在河北省石家庄市正定县、辽宁省鞍山市立山区、湖南省岳阳市岳阳县、厦门市海沧区和集美区5个区/县共计18个监测点招募研究对象并随访其子代自出生至3岁。研究纳入标准为:孕晚期(孕28~36周),单胎,在监测点建立过《孕产妇保健手册》,无精神疾患且自愿签署知情同意,共纳入2 731名研究对象。本研究排除标准包括:(1)孕妇孕前体重、膳食、孕期疾病情况等重要信息缺失者(39人);(2)早产儿及低出生体重儿(134人);(3)婴儿患有先天心脏病、畸形等严重影响儿童体格发育的疾病(11人);(4)0~3岁内体格检测信息<3次(76人);(5)婴儿分娩方式、喂养情况等重要信息缺失者(141人)。在进行研究人群的排除后,研究最终纳入2 330对母婴对。
二、调查内容与方法
1.数据收集:采用自制的《孕妇健康状况调查表》、《儿童随访调查表》和医疗/保健记录收集孕妇相关信息和儿童随访资料。本研究纳入的变量有48个,包括从《孕妇健康状况调查表》中获取的孕妇人口学信息(所属地区、家庭居住环境、家庭年收入、受教育程度、职业、怀孕时年龄),产次,孕期疾病(妊娠糖尿病、妊娠高血压综合征),孕期微量营养素摄入(叶酸、钙剂、铁剂、维生素),孕期生活行为习惯(吸烟、二手烟接触、孕晚期睡眠质量、孕晚期户外运动时长),孕晚期零食摄入及配偶体格信息。从《儿童随访调查表》中获取婴幼儿6月龄主要照顾者信息,喂养信息(母乳喂养时长,纯母乳喂养时长,辅食添加月龄,6月龄是否吃鱼虾、水果、蔬菜、肉类、谷类、吃豆制品、内脏,6月龄是否喝奶类、补充维生素D),疾病信息(1月龄是否住院,6月龄是否住院,6月龄内是否因感冒、腹泻、肺炎、发热住院),生活行为方式(1月龄睡眠时长、睡眠质量,6月龄睡眠时长、睡眠质量,6月龄与照顾者玩耍时长,室外活动时长)。从医疗/保健记录中摘录孕妇孕前体格信息,婴幼儿性别、分娩方式。
2.婴幼儿体格指标:婴幼儿出生时身长和体重信息摘录于产科病历/保健记录;1、6、12、18、24、30、36月龄时身长(身高)和体重信息由经过专业技术培训的健康检查人员,采用统一测量工具和测量方法所得,体重记录以千克(kg)为单位,读取至小数点后1位,身长(身高)记录以厘米(cm)为单位,读取至小数点后1位。
3.相关指标定义:(1)体质量指数(body mass index,BMI)= 体重(kg)/身高2(m2)。参考中国成人体质量指数[29]将婴幼儿母亲及父亲BMI分为消瘦(<18.5 kg/m2),正常体重(18.5~23.9 kg/m2),超重(24~27.9 kg/m2),肥胖(≥28 kg/m2)。(2)婴幼儿Z-BMI。按照WHO(2006年版)儿童体格发育评价标准,使用STATA 14.0软件,按照性别和年龄计算婴幼儿每个时点的Z-BMI[30]。(3)母乳喂养时长。参考中国婴幼儿与营养指南推荐[31],将婴幼儿母乳持续时间分为<6月、6~11月和≥12月;纯母乳喂养持续时间分为从未母乳喂养、0~5月和≥6月;将婴幼儿辅食添加月龄分为<4月、4~6月和>6月。
三、统计学方法
研究使用STATA 14.0软件进行统计分析。符合正态分布的连续型变量,以![]() 表示;分类资料采用构成比/率表示。
表示;分类资料采用构成比/率表示。
采用GBTM分析0~3岁婴幼儿的体格发育轨迹,Z-BMI为评价指标。该模型采用半参数轨迹分组策略,假设总体中存在多个潜在的轨迹,模型可拟算出每个个体属于不同轨迹的后验概率,以个体最大后验概率对应的增长轨迹作为分组依据,实现群体聚类。每个潜在的轨迹代表一个亚类,不同亚类的增长模式不同,但有限亚组中各个体变化的轨迹和截距是一致的,该模型弥补了传统的增长模型在探讨群体异质性方面的不足。研究从初始模型(假设只存在一个潜类别)开始拟合,逐渐增加潜类别数量;每个潜类别轨迹从五阶函数开始拟合,高阶不显著时继续拟合低阶项。基于贝叶斯信息准则(Bayesian information criteria,BIC)、调整贝叶斯信息准则(adjust BIC,aBIC)及赤池信息准则(Akaike information criterion,AIC)、模型可揭示数据的重要特征、模型简约性(各亚组最小样本量至少为5%的样本)对GBTM模型进行选择,BIC、aBIC、AIC三者为评价模型复杂度和拟合数据优良性的标准,其绝对值越低,模型拟合越好[32-33]。基于平均后验概率(average posterior probability,AvePP)对模型进行评价,用于判断模型是否真实反映样本数据,其越接近1越好,研究将0.70作为模型可接受的标准。
采用Group Lasso回归从48项潜在影响因素中筛选婴幼儿体格发育轨迹的影响因素,选择10折交叉验证法及模型误差最小加一个标准误时对应的参数λ值(λ.min)为最优调整参数。Lasso回归方法的本质是一种压缩估计,通过构造一个惩罚函数将某些变量的回归系数压缩至零,实现变量的有效选择,可解决传统模型中变量高度相关的问题,Group Lasso法是Lasso法的扩展,是以组为单位对数据进行选择,可以把一个指标设置的哑变量视为一组,同时选入模型或同时剔除[34]。
采用无序多分类Logistic回归模型分析不同体格发育轨迹的影响因素。以双侧P<0.05为差异有统计学意义。
结 果
一、基本情况
2 330个研究对象中,来自于南方人数占比56.0%(1 304/2 330),男童占比53.8%(1 253/2 330),自然分娩人数占比52.7%(1 227/2 330)。6月龄前,母亲为主要照顾者的婴儿占比89.8%(2 093/2 330),6月龄室外活动≥3 h者占比26.4%(615/2 330),母乳喂养时长<6、6~11、≥12月龄的婴儿比例分别为12.6%(294/2 330)、33.0%(768/2 330)、54.4%(1 267/2 330);辅食添加月龄为4~6月龄最多,占比70.6%(1 644/2 330)。婴幼儿母亲怀孕时平均年龄为(29.1±4.3)岁,经产妇占比53.6%(1 250/2 330),孕前消瘦、正常体重、超重及肥胖的比例分别为18.8%(438/2 330)、62.4%(1 454/2 330)、13.7%(320/2 330)、5.1%(118/2 330)。婴幼儿父亲体格为消瘦、正常体重、超重及肥胖的比例分别为4.4%(102/2 330)、50.2%(1 170/2 330)、33.6%(784/2 330)、11.8%(274/2 330),详见表1。
表1 研究对象(母婴)基本特征
Table 1 Baseline characteristics of 2 300 maternal-child dyads
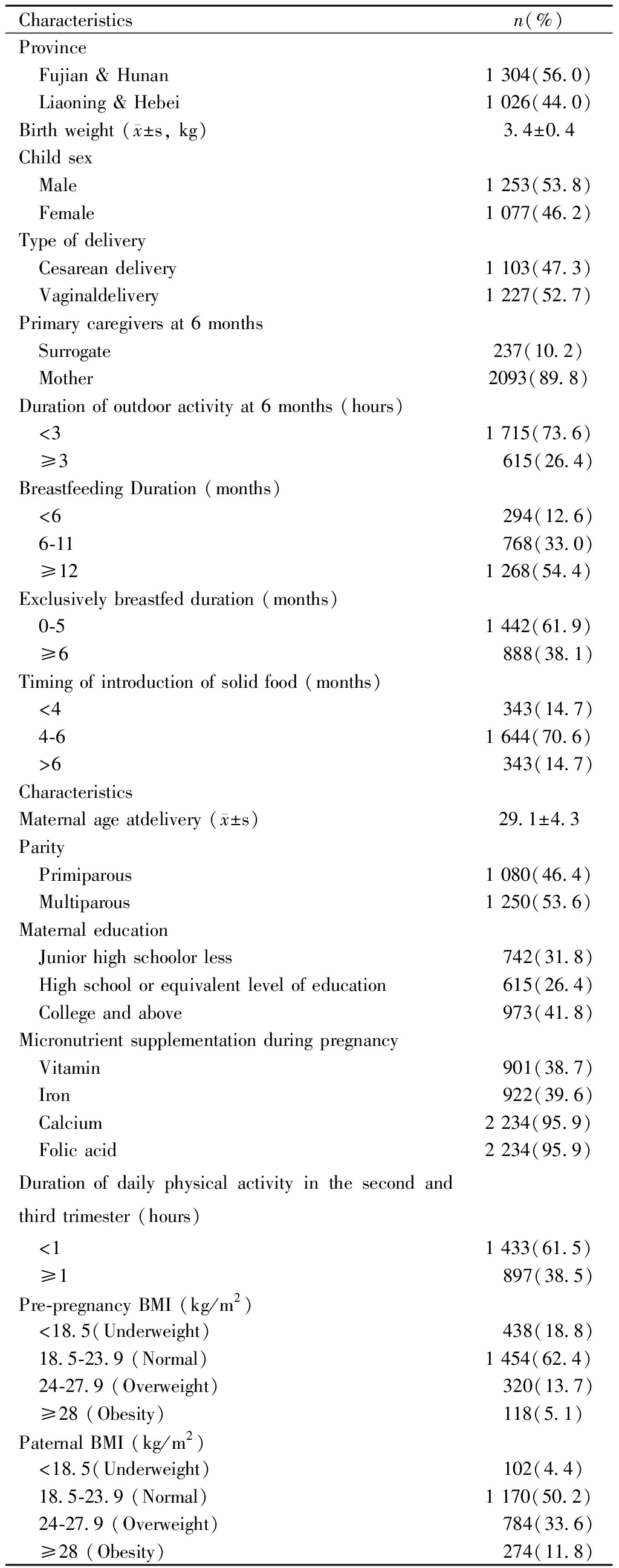
Characteristicsn(%)Province Fujian & Hunan1 304(56.0) Liaoning & Hebei1 026(44.0)Birth weight ( x±s, kg)3.4±0.4Child sex Male1 253(53.8) Female1 077(46.2)Type of delivery Cesarean delivery1 103(47.3) Vaginaldelivery1 227(52.7)Primary caregivers at 6 months Surrogate237(10.2) Mother2093(89.8)Duration of outdoor activity at 6 months (hours) <31 715(73.6) ≥3 615(26.4)Breastfeeding Duration (months) <6 294(12.6) 6-11 768(33.0) ≥121 268(54.4)Exclusively breastfed duration (months) 0-51 442(61.9) ≥6 888(38.1)Timing of introduction of solid food (months) <4 343(14.7) 4-61 644(70.6) >6 343(14.7)CharacteristicsMaternal age atdelivery ( x±s)29.1±4.3Parity Primiparous1 080(46.4) Multiparous1 250(53.6)Maternal education Junior high schoolor less 742(31.8) High school or equivalent level of education 615(26.4) College and above 973(41.8)Micronutrient supplementation during pregnancy Vitamin 901(38.7) Iron 922(39.6) Calcium2 234(95.9) Folic acid2 234(95.9)Duration of daily physical activity in the second and third trimester (hours) <11 433(61.5) ≥1 897(38.5)Pre-pregnancy BMI (kg/m2) <18.5(Underweight) 438(18.8) 18.5-23.9 (Normal)1 454(62.4) 24-27.9 (Overweight) 320(13.7) ≥28 (Obesity)118(5.1)Paternal BMI (kg/m2) <18.5(Underweight)102(4.4) 18.5-23.9 (Normal)1 170(50.2) 24-27.9 (Overweight) 784(33.6) ≥28 (Obesity) 274(11.8)
Abbreviation:BMI, body mass index.
二、婴幼儿不同生长轨迹的GBTM模型分析
潜在类别组数(亚组数)从1增加至5时,AIC、BIC及a-BIC不断减小,但亚组数为5组时,其中一组内样本量过低(低于总样本量5%)。AIC、BIC及模型简约原则提示亚组数为4组时,模型优拟合最优;并且4组的AvePP分别为0.92,0.79,0.84,0.91,均大于经验标准0.70,认为模型拟合情况较好,模型拟合信息汇总见表2。
表2 1~5组潜在类别模型拟合信息汇总
Table 2 Information criteria for trajectory models with 1-5 classes
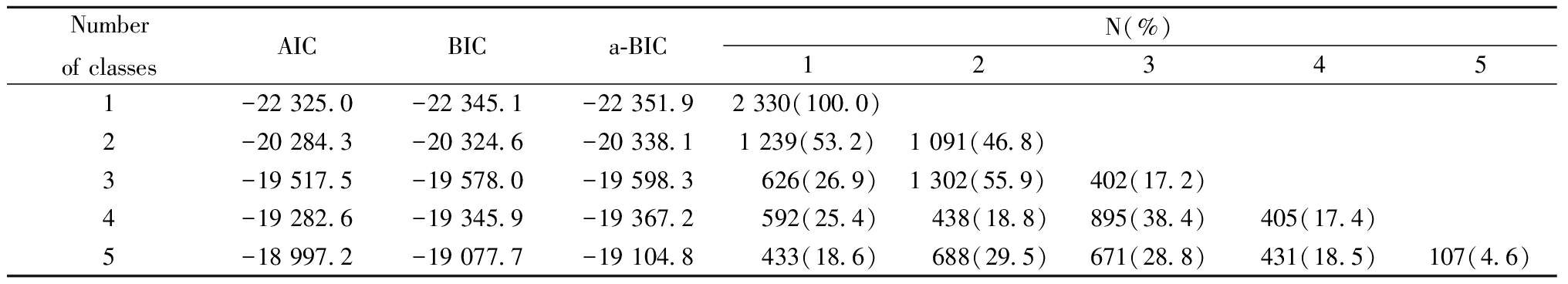
Number of classesAICBICa-BICN(%)123451-22 325.0-22 345.1-22 351.92 330(100.0)2-20 284.3-20 324.6-20 338.11 239(53.2)1 091(46.8)3-19 517.5-19 578.0-19 598.3 626(26.9)1 302(55.9)402(17.2)4-19 282.6-19 345.9-19 367.2 592(25.4) 438(18.8)895(38.4)405(17.4)5-18 997.2-19 077.7-19 104.8 433(18.6) 688(29.5)671(28.8)431(18.5)107(4.6)
Abbreviation:AIC:Akaike Information Criterion.BIC:Bayesian Information Criterion.a-BIC:adjusted BIC.
第1组占比25.4%(592/2 330),该组婴幼儿初始Z-BMI均值为(-0.5±0.9),低于平均水平(-0.1±1.0),0~36月龄Z-BMI呈现稳定缓慢下降趋势(β=-0.01,P <0.05),将其定义为缓慢生长组。第2组占比18.8%(438/2 330),该组婴幼儿初始Z-BMI均值最低,为(-1.3±0.6),Z-BMI在0~6月龄间呈现快速增长趋势(β=0.55,P <0.05),6月龄达最高点后缓趋于正常且平稳状态,将其定义为追赶生长组。第3组占比38.4%(895/2 330),该组婴幼儿初始Z-BMI均值为(0.5±0.7),Z-BMI 0~6月龄间呈现缓慢增长趋势(β=0.02,P<0.05),6月龄达最高点后缓趋于正常且平稳状态,将其定义为中速生长组。第4组占比17.4%(405/2 330),该组婴幼儿初始Z-BMI均值为(0.3±0.9),略高于平均水平,Z-BMI在出生至6月龄间呈现快速增长趋势(β=0.52,P<0.05),6月龄达最高点后缓趋于正常且平稳状态,将其定义为加速生长组。见图1a、图1b。
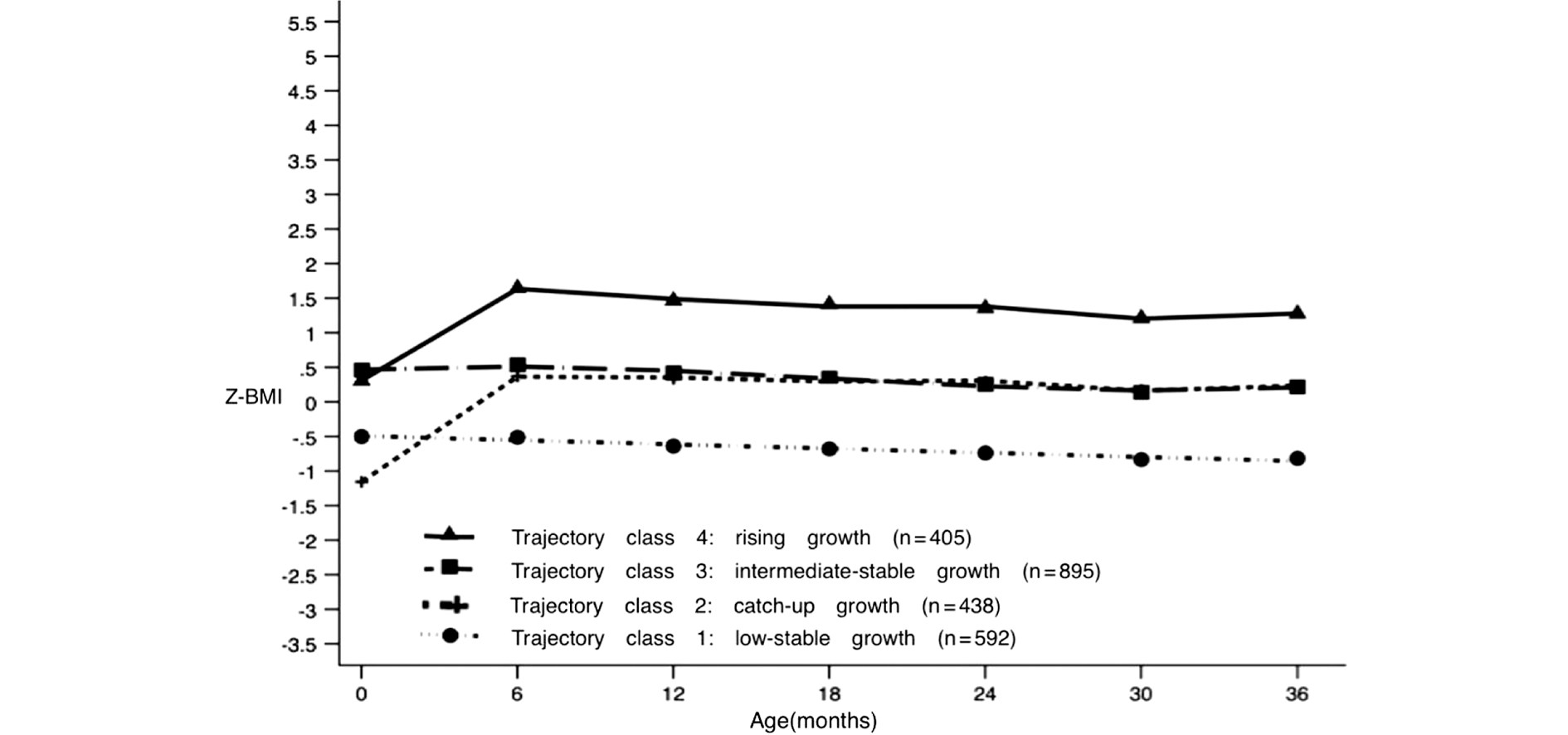
图1a 0~3岁婴幼儿ZBMI生长轨迹图(基于群组轨迹模型)
Figure 1a The trajectories of body mass index z-score(Z-BMI)in the first 3 years of age according to GBTM

图1b 0~3岁婴幼儿ZBMI生长轨迹图
Figure 1b Summary of four z-BMI growth trajectory groups
Note:Solid line in each plot indicates the mean trajectory of the corresponding group
三、不同生长轨迹的影响因素分析
在研究初期纳入的48个变量中,通过Group Lasso回归最终筛选出10个与婴幼儿体格发育轨迹相关性显著的变量,包括家庭收入,父亲体格,母亲孕前体格、孕晚期户外运动时长、孕期是否服用铁剂,婴儿出生体重、分娩方式、1月龄睡眠质量、6月龄室外活动时长、纯母乳喂养时长。选择10折交叉验证法及模型误差最小加一个标准误时对应的参数λ值(λ.min)为最优调整参数,最终在λ取值0.04[logλ=-3.22]时获得具备优良性且自变量个数最少的模型,见图2。
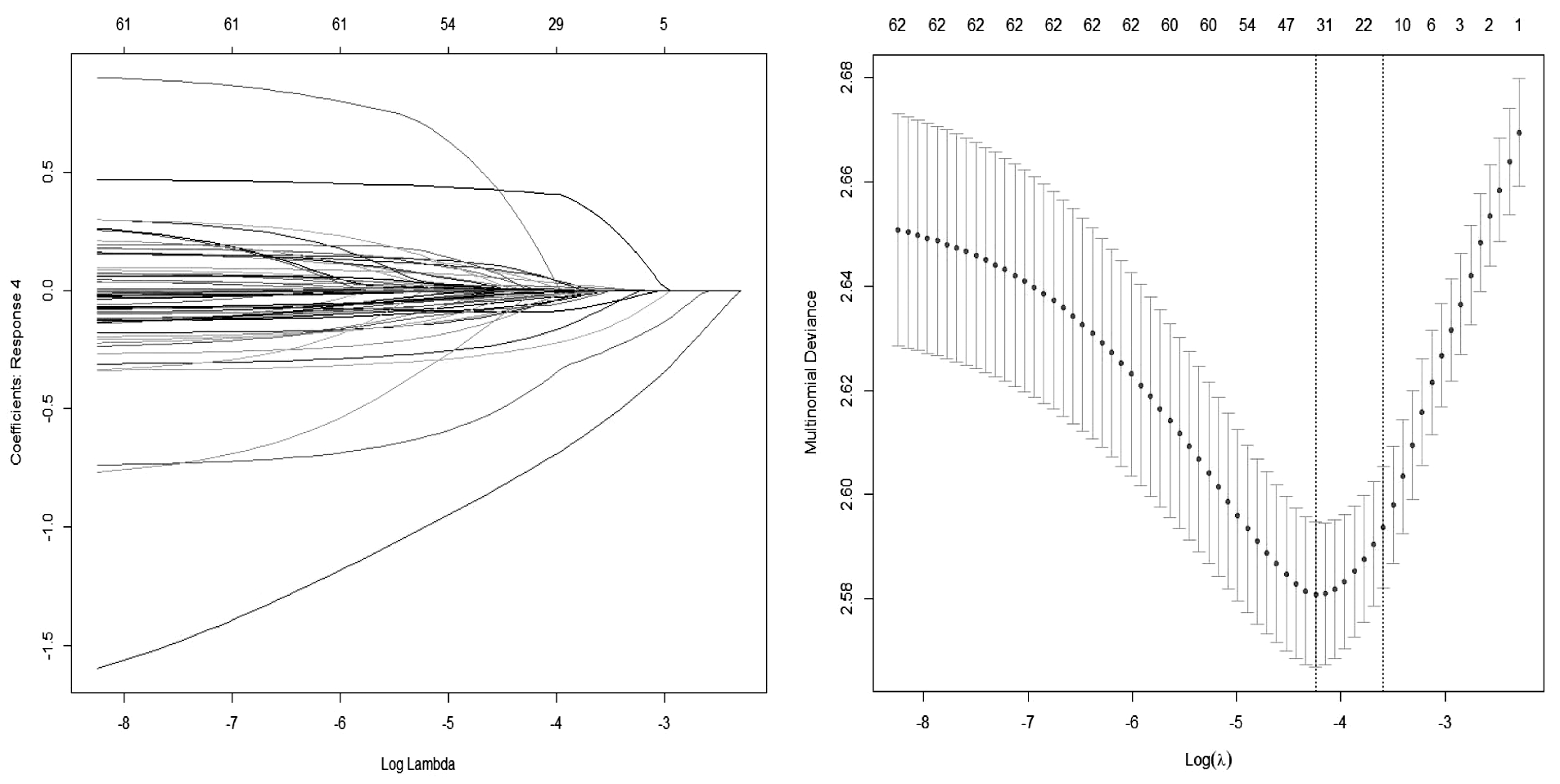
图2 基于group lasso回归的特征性变量筛选
Figure 2 Candidate variable selection using LASSO regression
以婴幼儿体格发育轨迹为因变量,Group Lasso回归筛选的10个变量为自变量,调整地区及婴幼儿性别,以中速生长组作为参考,经无序多分类Logistic回归分析发现:父亲消瘦,母亲孕前消瘦,孕晚期户外运动时长小于1 h,孕期未服用铁剂及6月龄室外活动时长<3 h的婴幼儿是缓慢生长的危险因素,OR(95%CI)值分别为1.80(1.08~3.01),1.61(1.23~2.11),1.30(1.04~1.63),1.47(1.17~1.85)及1.36(1.06~1.75);父亲超重、肥胖,母亲孕前超重,出生体重≥4 kg、1月龄时睡眠质量好可显著降低缓慢生长模式的发生风险,OR(95%CI)值分别0.56(0.43~0.71)、0.68(0.47~0.99)、0.59(0.40~0.85)、0.27(0.16~0.45)、0.74(0.58~0.94);纯母乳喂养时长<6个月是追赶生长的危险因素,OR(95%CI)值为1.37(1.07~1.76);母亲孕前肥胖,剖宫产,纯母乳喂养时长<6个月是加速生长模式的危险因素,OR(95%CI)值分别为1.69(1.07~2.66),1.43(1.12~1.83),1.39(1.07~1.79)。详见表3。
表3 产前及产后因素对婴幼儿ZBMI轨迹的影响
Table 3 Association of prenatal and postnatal factors with child′s Z-BMI trajectories
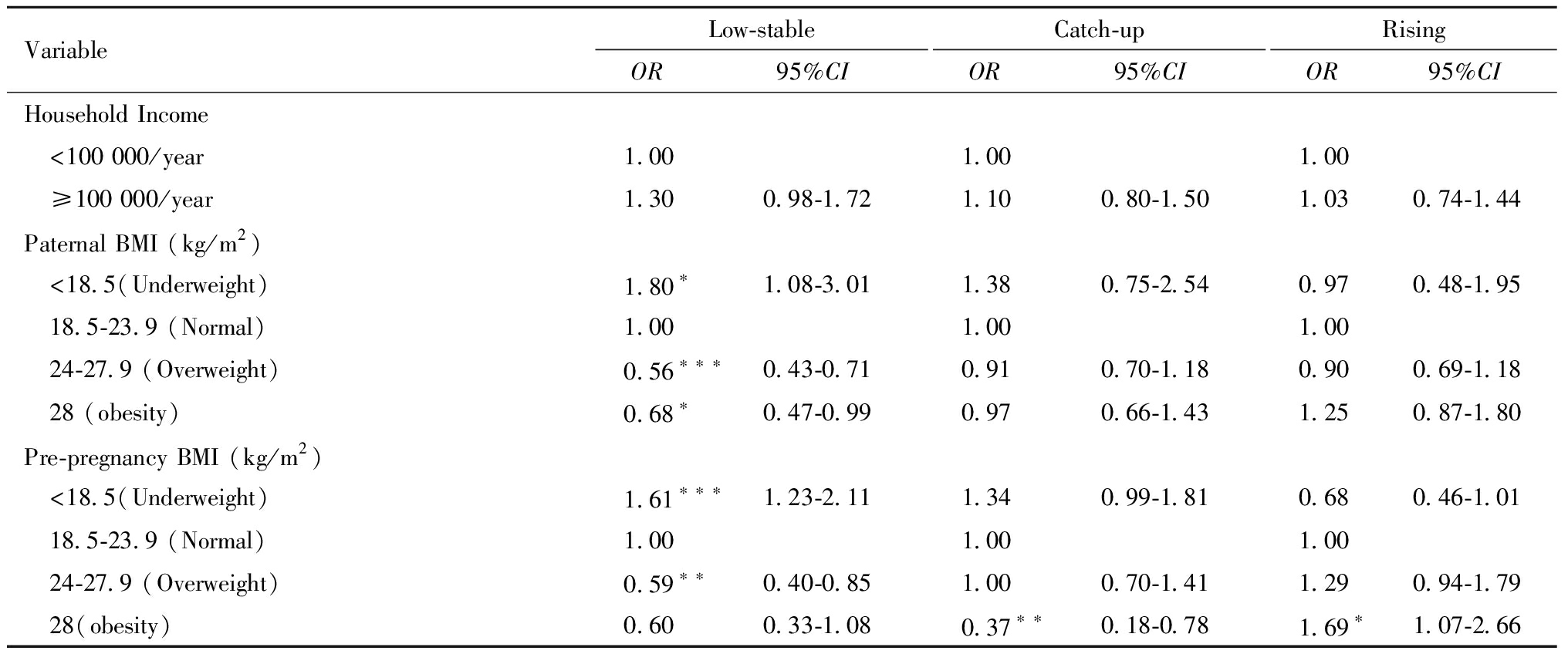
VariableLow-stableOR95%CICatch-upOR95%CIRisingOR95%CIHousehold Income <100 000/year1.001.001.00 ≥100 000/year1.300.98-1.721.100.80-1.501.030.74-1.44Paternal BMI (kg/m2) <18.5(Underweight)1.80∗1.08-3.011.380.75-2.540.970.48-1.95 18.5-23.9 (Normal)1.001.001.00 24-27.9 (Overweight)0.56∗∗∗0.43-0.710.910.70-1.180.900.69-1.18 28 (obesity)0.68∗0.47-0.990.970.66-1.431.250.87-1.80Pre-pregnancy BMI (kg/m2) <18.5(Underweight)1.61∗∗∗1.23-2.111.340.99-1.810.680.46-1.01 18.5-23.9 (Normal)1.001.001.00 24-27.9 (Overweight)0.59∗∗0.40-0.851.000.70-1.411.290.94-1.79 28(obesity)0.600.33-1.080.37∗∗0.18-0.781.69∗1.07-2.66
表3(续)
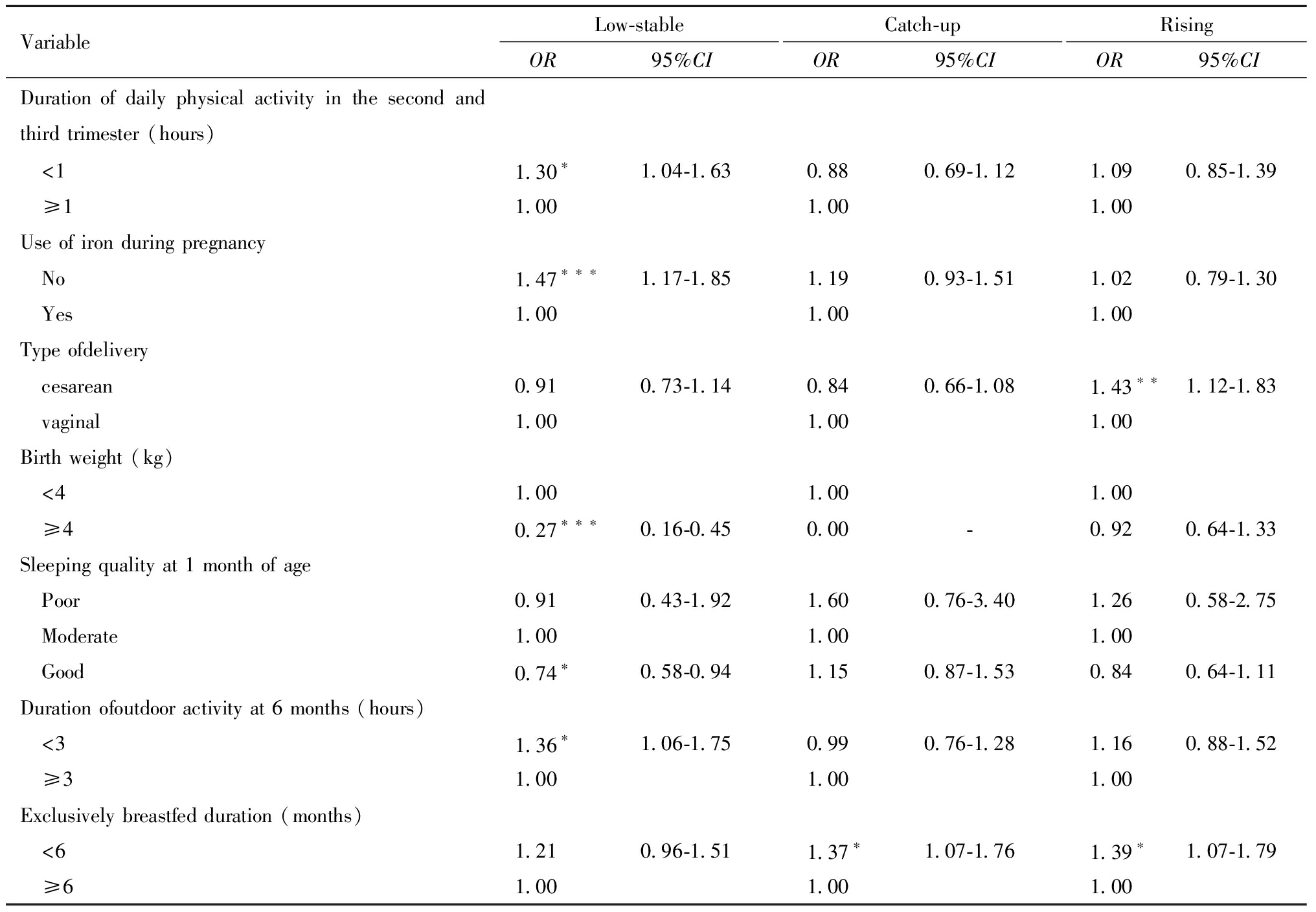
VariableLow-stableOR95%CICatch-upOR95%CIRisingOR95%CIDuration of daily physical activity in the second and third trimester (hours) <1 1.30∗1.04-1.630.880.69-1.121.090.85-1.39 ≥1 1.001.001.00Use of iron during pregnancy No1.47∗∗∗1.17-1.851.190.93-1.511.020.79-1.30 Yes1.001.001.00Type ofdelivery cesarean0.910.73-1.140.840.66-1.081.43∗∗1.12-1.83 vaginal1.001.001.00Birth weight (kg) <4 1.001.001.00 ≥4 0.27∗∗∗0.16-0.450.00-0.920.64-1.33Sleeping quality at 1 month of age Poor0.910.43-1.921.600.76-3.401.260.58-2.75 Moderate1.001.001.00 Good0.74∗0.58-0.941.150.87-1.530.840.64-1.11Duration ofoutdoor activity at 6 months (hours) <3 1.36∗1.06-1.750.990.76-1.281.160.88-1.52 ≥3 1.001.001.00Exclusively breastfed duration (months) <6 1.210.96-1.511.37∗1.07-1.761.39∗1.07-1.79 ≥6 1.001.001.00
*P<0.05,**P<0.01, ***P<0.001.
Abbreviation:BMI:body mass index.OR:Odds ratios.95%CI:95% confidence intervals.Reference group for outcome is the intermediate-stable growth trajectory.
讨 论
本研究将婴幼儿体格发育轨迹分为缓慢生长、追赶生长、中速生长和加速生长组(占比分别为25.4%、18.8%、38.4%和17.4%),4种生长轨迹在出生至6月龄间出现了明显差异,随后在6至36月龄间的保持平稳状态。多因素分析发现,父亲消瘦、母亲孕前消瘦、母亲孕晚期户外运动时长小于1 h、孕期未服用铁剂、6月龄室外活动时长<3 h与婴幼儿缓慢生长相关;母亲孕前肥胖、剖宫产、纯母乳喂养时长小于6个月与婴幼儿加速生长相关。
现有关于3岁以下婴幼儿体格发育轨迹的研究,基于GBTM分析发现的轨迹数多为4个(范围为3~7)[24-25, 27-28, 35]。Giles等学者聚焦于澳大利亚出生至3.5岁婴幼儿的体格发育状况,研究确定了低速、中速、高速和加速生长4条Z-BMI生长轨迹,并发现4条轨迹尤其在 6月龄内差异最为明显[24],与本研究结果一致。多名学者[23, 28, 36]也发现,婴幼儿的生长发育轨迹在最初6月龄内差异较大,提示婴幼儿体格发育轨迹模式具有一定的相似性,并且未来研究可重点关注婴幼儿出生6月龄内的生长轨迹。
0~3岁的婴幼儿体格发育及其发育轨迹的差异对个体的影响可能会延续到儿童、青少年乃至成年期[1-8, 24, 37]。因此,确定各个轨迹的影响因素也十分重要。目前探讨婴幼儿体格发育轨迹影响因素的研究有限且结论尚未统一。Giles[24]等研究者将婴幼儿分成了低、中、高及加速增长,发现孕早期母体肥胖、孕期增重超过10 kg、经产妇是婴幼儿处于加速增长的危险因素。Aris [35]等研究者发现母体肥胖、孕期过度增重(参照2009年美国医学研究所指南),马来人和印度人种族是高稳定和加速生长模式的危险因素,早产和印度种族是缓慢生长组的危险因素。Slining[25]等研究者发现,母亲身高、肥胖程度、胎次、严重呼吸道感染等因素与婴幼儿BMI轨迹相关。但Kwon[23]等研究者发现不同的轨迹组与婴幼儿性别,孕产妇种族、教育和家庭收入之间无统计学关联。
本研究发现,父亲体格状况与婴幼儿Z-BMI生长轨迹相关,父亲消瘦可增加婴幼儿缓慢生长风险,超重、肥胖则与缓慢生长风险下降有关。父亲的体格发育状况可能通过父系表观遗传修饰遗传给后代,一项研究显示,男性的体重会对其精子中可遗传信息进行修饰,从而影响下一代的体格状况[38];此外,父亲的体格状况受到家庭环境的影响,父亲饮食生活习惯可能也会对婴幼儿产生一定的影响[39]。母亲的体格状况也与婴幼儿Z-BMI生长轨迹相关,其中孕前消瘦是婴幼儿缓慢生长的危险因素,超重是缓慢生长的保护因素,肥胖是加速生长的危险因素,这与Giles[24],Liu[28]等的研究一致,这些关联可由母亲及其子代间共享遗传和环境因素来解释[39-40]。本研究发现剖宫产为婴幼儿加速生长的危险因素,这与Zhang等[41]研究者的结果一致,Zhang等人的研究是第一个分析分娩方式与婴幼儿Z-BMI轨迹关联的研究,该研究发现孕妇选择性和非选择性剖宫产会增加婴幼儿Z-BMI加速体格发育轨迹的风险[41],这可能与新生儿出生时首次接触的微生物群有关[42]。
研究还发现孕中晚期户外运动时长<1 h、婴幼儿6月龄室外活动时长<3 h均为婴幼儿缓慢生长的危险因素,这可能是因缺乏维生素D所致,体内所需的90%维生素D来源于日光或紫外线照射皮肤产生,外出时间少即减少了孕妇及其子代的日照时间,可能导致婴幼儿维生素D缺乏[43-44]。赵艳[45]等学者的研究发现,孕期每天户外活动时间<1 h的母亲其子代患维生素D缺乏的风险增加1.71倍。孕期服用铁剂也是婴幼儿生长轨迹的影响因素,孕期铁缺乏可能会增加促肾上腺皮质激素释放激素及皮质醇的生成,造成胎儿红细胞氧化损伤,可能会抑制胎儿的成长[46],Cogswell等对513名低收入孕妇进行的随机对照实验显示,孕期服用铁剂的孕妇后代平均出生体重显著增加,低出生体重率显著降低[47]。婴幼儿出生后的行为习惯、母乳喂养情况也与Z-BMI轨迹也有一定的关联,1月龄睡眠质量好是缓慢生长的保护因素,早期探讨婴幼儿睡眠质量与体格发育关联的研究也发现睡眠质量好可有效改善婴幼儿的体格发育状态[48-49]。此外,坚持纯母乳喂养小于6个月,是婴幼儿处于加速生长的危险因素,纯母乳喂养时间短提示婴幼儿过早引入辅食,这与先前的研究一致[50-51]。
本研究为大样本量前瞻性队列研究,包含婴幼儿体格测量的多次随访数据,并且包含社会人口学、孕妇生活行为习惯、婴幼儿生活行为习惯等多方面数据,为纵向分析婴幼儿体格发育轨迹及探讨其影响因素提供了有效的样本量;婴幼儿体格发育及其发育轨迹受到环境和遗传因素的作用,这些影响因素之间关系复杂,且存在着一定的相关性,而现有探讨婴幼儿发育轨迹影响因素的研究采用Logistic回归、卡方检验等传统的统计分析方法[24-25, 27-28, 35],可能存在估计偏差,难筛选出最有意义的变量,本研究选择采用group lasso回归进行潜在影响因素的筛选,可有效解决纳入多项影响因素时多重共线性的问题,在此基础上,本研究首次发现了孕中晚期户外运动时间、婴幼儿6月龄室外活动时长、孕期服用铁剂等因素与婴幼儿生长轨迹之间的关联。但是本研究也存在一些不足。首先,较多潜在影响因素的纳入增加了数据缺失的概率,剔除缺失的数据后,样本量会随之减少,或会产生一定的误差,未来需要考虑如何合理地选择纳入模型的因素,在误差较小的情况下保证最好的样本量。其次,研究缺乏能体现婴幼儿子宫内发育的数据,比如妊娠期体重变化情况等,这些因素可能影响出生后的生长轨迹,因此在进行多项式Logistic回归模型评价影响因素时,无法针对某些潜在的混杂因素进行充分调整。最后,本研究中婴幼儿睡眠质量、睡眠时长等指标是由照顾者主观评价,可能会带来一些报告偏倚,未来需要通过更严谨设计的研究进一步调查婴幼儿早期生长的复杂影响因素。
结 论
本研究通过纵向队列研究,采用GBTM在婴幼儿出生至3岁内确定了4条体格发育轨迹,其中出生至6月龄间轨迹变化出现不同趋势;父亲消瘦,母亲孕前消瘦、孕晚期户外运动时长小于1 h、孕期未补充铁剂,6月龄室外活动时长<3 h可增加婴幼儿缓慢生长的风险;母亲孕前肥胖,剖宫产,纯母乳喂养时长小于6个月可增加婴幼儿加速生长的风险,这为促进婴幼儿健康发育提供了科学证据。
1 Ong KK,Emmett P,Northstone K,et al.Infancy weight gain predicts childhood body fat and age at menarche in girls.J Clin Endocrinol Metab,2009,94:1527-1532.
2 Druet C,Stettler ER,Sharp S,et al.Prediction of childhood obesity by infancy weight gain:an individual-level meta-analysis.Paediatr Perinat Epi,2012,26:19-26.
3 Stettler N,Iotova V.Early growth patterns and long-term obesity risk.Curr Opin Clin Nutr Metab Care,2010,13:294-299.
4 Geserick M,Vogel M,Gausche R,et al.Acceleration of BMI in early childhood and risk of sustained obesity.New Engl J Med,2018,379:1303-1312.
5 Perng W,Rifas-Shiman SL,Kramer MS,et al.Early weight gain,linear growth,and mid-childhood blood pressure:A prospective study in project viva.Hypertension(Dallas,Tex :1979),2016,67:301-308.
6 Woo BJ,Locks LM,Cheng ER,et al.Risk factors for childhood obesity in the first 1,000 days:A systematic review.Am J Prev Med,2016,50:761-779.
7 Ong KK,Loos RJ.Rapid infancy weight gain and subsequent obesity:systematic reviews and hopeful suggestions.Acta Paediatr,2006,95:904-908.
8 Ekelund U,Ong KK,Linne Y,et al.Association of weight gain in infancy and early childhood with metabolic risk in young adults.J Clin Endocrinol Metab,2007,92:98-103.
9 Richter LM,Daelmans B,Lombardi J,et al.Investing in the foundation of sustainable development:pathways to scale up for early childhood development.Lancet,2017,389:103-118.
10 Ong KK,Ahmed ML,Dunger DB,et al.Association between postnatal catch-up growth and obesity in childhood:Prospective cohort study.Brit Med J,2000,320:967-971.
11 Reilly JJ,Armstrong J,Dorosty AR,et al.Early life risk factors for obesity in childhood:Cohort study.BMJ,2005,330:1357-1369.
12 Nagin DS,Odgers CL.Group-based trajectory modeling in clinical research.Annu Rev Clin Psychol,2010,6:109-138.
13 Herle M,Micali N,Abdulkadir M,et al.Identifying typical trajectories in longitudinal data:modelling strategies and interpretations.Eur J Epidemiol,2020,35:205-222.
14 Haga C,Kondo N,Suzuki K,et al.Developmental trajectories of body mass index among japanese children and impact of maternal factors during pregnancy.PLoS ONE,2012,7:e51896.
15 Ziyab AH,Karmaus W,Kurukulaaratchy RJ,et al.Developmental trajectories of body mass index from infancy to 18 years of age:prenatal determinants and health consequences.J Epidemiol Commun H,2014,68:934-941.
16 Magee CA,Caputi P,Iverson DC.Identification of distinct body mass index trajectories in Australian children.Pediatr Obes,2013,8:189-198.
17 Keating C,Backholer K,Gearon E,et al.Prevalence of class-I,class-II and class-III obesity in Australian adults between 1995 and 2011-12.Obes Res Clin Pract,2015,9:553-562.
18 Pryor LE,Tremblay RE,Boivin M,et al.Developmental trajectories of body mass index in early childhood and their risk factors:An 8-year longitudinal study.Arch Pediatr Adolesc Me,2011,165:906-912.
19 Tu AW,Masse LC,Lear SA,et al.Body mass index trajectories from ages 1 to 20:Results from two nationally representative canadian longitudinal cohorts.Obesity,2015,23:1703-1711.
20 Lane SP,Bluestone C,Buekr CT.Trajectories of BMI from early childhood through early adolescence:SES and psychosocial predictors.Brit J Health Psych,2013,18:66-82.
21 Mustillo S,Worthman C,Erkanli A,et al.Obesity and psychiatric disorder:Developmental trajectories.Pediatrics,2003,111:851-859.
22 Ventura AK,Loken E,Birch LL.Developmental trajectories of girls′ BMI across childhood and adolescence.Obesity,2009,17:2067-2074.
23 Kwon S,Janz KF,Letuchy EM,et al.Association between body mass index percentile trajectories in infancy and adiposity in childhood and early adulthood.Obesity,2017,25:166-171.
24 Giles LC,Whitrow MJ,Davies MJ,et al.Growth trajectories in early childhood,their relationship with antenatal and postnatal factors,and development of obesity by age 9 years:results from an Australian birth cohort study.Int J Obes,2015,39:1049-1056.
25 Slining MM,Herring AH,Popkin BM,et al.Infant BMI trajectories are associated with young adult body composition.J Dev Orig Hlth Dis,2013,4:56-68.
26 Ford ND,Martorell R,Mehta NK,et al.Life-course body mass index trajectories are predicted by childhood socioeconomic status but not exposure to improved nutrition during the first 1000 days after conception in guatemalan adults.J Nutr,2016,146:2368-2374.
27 Stout SA,Espel EV,Sandman CA,et al.Fetal programming of children′s obesity risk.Psychoneuroendocrinology,2015,53:29-39.
28 Liu JX,Liu J,Frongillo EA,et al.Body mass index trajectories during the first year of life and their determining factors.Am J Hum Biol,2019,31:10.1002/ajhb.23188.
29 中国肥胖问题工作组数据汇总分析协作组.我国成人体重指数和腰围对相关疾病危险因素异常的预测价值:适宜体重指数和腰围切点的研究.中国儿童保健杂志,2002,01:10-15.
30 GROUP.WMGRS.WHO Child Growth Standards:Length/height-for-age,weight-for-age,weight-for-length,weight-for-height and body mass index-for-age:Methods and development.Geneva:World Health Organization.2006.
31 婴幼儿喂养与营养指南.中国妇幼健康研究,2019,30:392-417.
32 Berlin KS,Parra GR,Williams NA.An introduction to latent variable mixture modeling(Part 2):longitudinal latent class growth analysis and growth mixture models.J Pediatr Psychol,2014,39:188-203.
33 冯国双,于石成,胡跃华.轨迹分析模型在流行病学研究中的应用.中华流行病学杂,2014,35:865-867.
34 Yuan M,Lin Y.Model selection and estimation in regression with grouped variables.J R Stat Soc B,2006,68:49-67.
35 Aris IM,Chen LW,Tint MT,et al.Body mass index trajectories in the first two years and subsequent childhood cardio-metabolic outcomes:a prospective multi-ethnic Asian cohort study.Sci Rep,2017,7:8424.
36 Montazeri P,Vrijheid M,Martinez D,et al.Maternal metabolic health parameters during pregnancy in relation to early childhood BMI trajectories.Obesity,2018,26:588-596.
37 Liu JX,Liu JH,Frongillo EA,et al.Body mass index trajectories during infancy and pediatric obesity at 6 years.Ann Epidemiol,2017,27:708-715.
38 Donkin I,Versteyhe S,Ingerslev L,et al.Obesity and bariatric surgery drive epigenetic variation of spermatozoa in humans.Cell Metab,2016,23:369-378.
39 Swinburn B,Egger G.Preventive strategies against weight gain and obesity.Obes Rev,2002,3:289-301.
40 Oken E,Gillman MW.Fetal origins of obesity.Obes Res,2003,11:496-506.
41 Zhang LH,Huang LX,Zhao ZY,et al.Associations between delivery mode and early childhood body mass index Z-score trajectories:A retrospective analysis of 2,685 children from mothers aged 18 to 35 years at delivery.Front Pediatr,2020,8:10.3389/fped.2020.598016.
42 Mueller NT,Whyatt R,Hoepner L,et al.Prenatal exposure to antibiotics,cesarean section and risk of childhood obesity.Int J Obes,2015,39:665-670.
43 Dawodu A,Davidson B,Woo JG,et al.Sun exposure and vitamin D supplementation in relation to vitamin D status of breastfeeding mothers and infants in the global exploration of human milk study.Nutrients,2015,7:1081-1093.
44 Thieden E,Philipsen PA,Heydenreich J,et al.Vitamin D level in summer and winter related to measured UVR exposure and behavior.Photochem Photobiol,2009,85:1480-1484.
45 赵艳,秦锐,秦振英,等.孕期户外活动时间与子代0~2岁婴幼儿维生素D状况的关系研究.中国妇幼保健,2019,34:4212-4215.
46 Gambling L,Kennedy C,Mcardle HJ.Iron and copper in fetal development.Semin Cell Dev Biol,2011,22:637-644.
47 Cogswell ME,Ibrahim P,Liza I,et al.Iron supplementation during pregnancy,anemia,and birth weight:a randomized controlled trial.Am J Clin Nutr,2003,78:773-781.
48 胡金梅,邓人武,彭向京.0~6月婴儿生长发育与睡眠状况的关系.中国生育健康杂志,2013,24:387-388.
49 Mihrshahi S,Gow ML,Baur LA.Contemporary approaches to the prevention and management of paediatric obesity:an Australian focus.Med J Australia,2018,209:267-274.
50 Carling SJ,Demment MM,Kjolhede CL,et al.Breastfeeding duration and weight gain trajectory in infancy.Pediatrics,2015,135:111-119.
51 Oddy WH,Mori TA,Huang RC,et al.Early infant feeding and adiposity risk:From infancy to adulthood.Ann Nutr Metab,2014,64:262-270.