双胎妊娠根据绒毛膜性可分为单绒毛膜(单绒)双胎和双绒毛膜(双绒)双胎,其中单绒双胎由于共用一个胎儿胎盘循环,具有发生某些严重妊娠并发症和子代不良结局的病理生理基础[1-2],研究显示单绒双胎较双绒双胎围产期死亡风险增高[3-7]。但由于既往早期影像学检查对双胎绒毛膜性的判断以及宫内畸形筛查水平的限制,对不同绒毛膜性双胎子代妊娠28周前流产(尤其是孕14周前早期流产)和出生缺陷缺乏良好统计数据。随着北京市早孕期超声筛查服务(包括对双胎绒毛膜性的判断)以及妊娠20~24周筛畸超声全面开展,单绒双胎和双绒双胎分别被列为妊娠风险因素登记在妇幼信息系统中并记录子代结局。本研究拟利用上述较完善的妇幼信息数据采集系统,对不同绒毛膜性双胎妊娠的子代结局开展全面分析,并探讨影响不同绒毛膜性双胎子代不良结局的危险因素。
对象与方法
一、研究对象
2020年1月1日至12月31日北京市妇幼保健网络信息系统《围产保健管理登记卡》中登记的孕产妇及其子代为研究对象。纳入标准:(1)孕妇早孕期超声(<14孕周,北京市早孕期胎儿畸形超声筛查时限为11~13+6孕周)提示双胎妊娠;(2)早孕期超声确认了绒毛膜性;(3)有明确妊娠结局。排除标准:(1)孕妇早孕期超声提示单胎或3胎及以上妊娠;(2)未行早孕期超声确认绒毛膜性;(3)无明确妊娠结局。最终纳入双胎妊娠孕妇2 872例,根据超声提示的双胎绒毛膜性,分为单绒双胎妊娠组(单绒组,n=642,22.4%)和双绒双胎妊娠组(双绒组,n=2 230,77.6%)。
二、研究方法
1. 资料收集:本研究为回顾性队列研究,资料来源于北京市妇幼保健网络信息系统《围产保健管理登记卡》中登记的信息,包括孕妇年龄、民族、孕次、产次、孕前BMI,既往不孕、自然流产、胎死宫内、胎儿畸形等不良孕产史,子宫肌瘤、子宫纵隔、残角子宫等子宫畸形或各类子宫手术史等子宫异常情况,受孕方式、妊娠合并症/并发症、妊娠结局、子代出生缺陷等。本研究遵循的程序符合本院伦理委员会规定,通过该伦理委员会批准(审批文号:2018-KY-039-01)。
2. 指标定义:以早孕期超声显示的孕囊、胎盘数量、胎膜与胎盘插入点“T”征和“λ”征进行双胎及其绒毛膜性的确认。结局指标包括子代<28孕周流产、围产期死亡(≥28孕周死胎死产、生后7日内早期新生儿死亡)和出生缺陷(监测期限为孕13周至生后1年)的发生;其中胎儿死亡孕周(或早期新生儿死亡的出生孕周)又分别按照<14孕周、14~27孕周、28~33孕周和≥34孕周进行进一步区分。
3. 统计学方法:采用SPSS 18.0软件对数据进行统计学分析,分析方法包括描述性分析单绒组和双绒组孕母的特征和子代不良结局,对两组间差异进行比较,并对影响不同绒毛膜双胎子代不良结局的危险因素进行多因素分析。计数资料采用频数及百分率表示,两组间的比较采用χ2检验或连续校正χ2检验,多因素分析采用二元Logistic回归模型分析。以P<0.05(双侧检验)为差异有统计学意义。
结 果
一、不同绒毛膜性双胎妊娠孕妇的临床特征
单绒组孕妇与双绒组孕妇相比,35岁以上(20.1% vs. 27.8%)、首次妊娠(41.4% vs. 54.6%)、首次分娩(84.4% vs. 89.1%)、辅助生殖技术受孕(10.3% vs. 55.8%)、既往不良孕产史(3.0% vs. 6.4%)、孕前BMI≥24.0(23.6% vs. 27.7%)的比例较低(P<0.05);少数民族、子宫异常以及合并/并发高血压、糖尿病和贫血的差异无统计学意义(P>0.05),结果见表1。
表1 不同绒毛膜性双胎妊娠孕妇的临床特征 [例(%)]
Table 1 Characteristics of pregnant women with different twin chorionicity [n(%)]
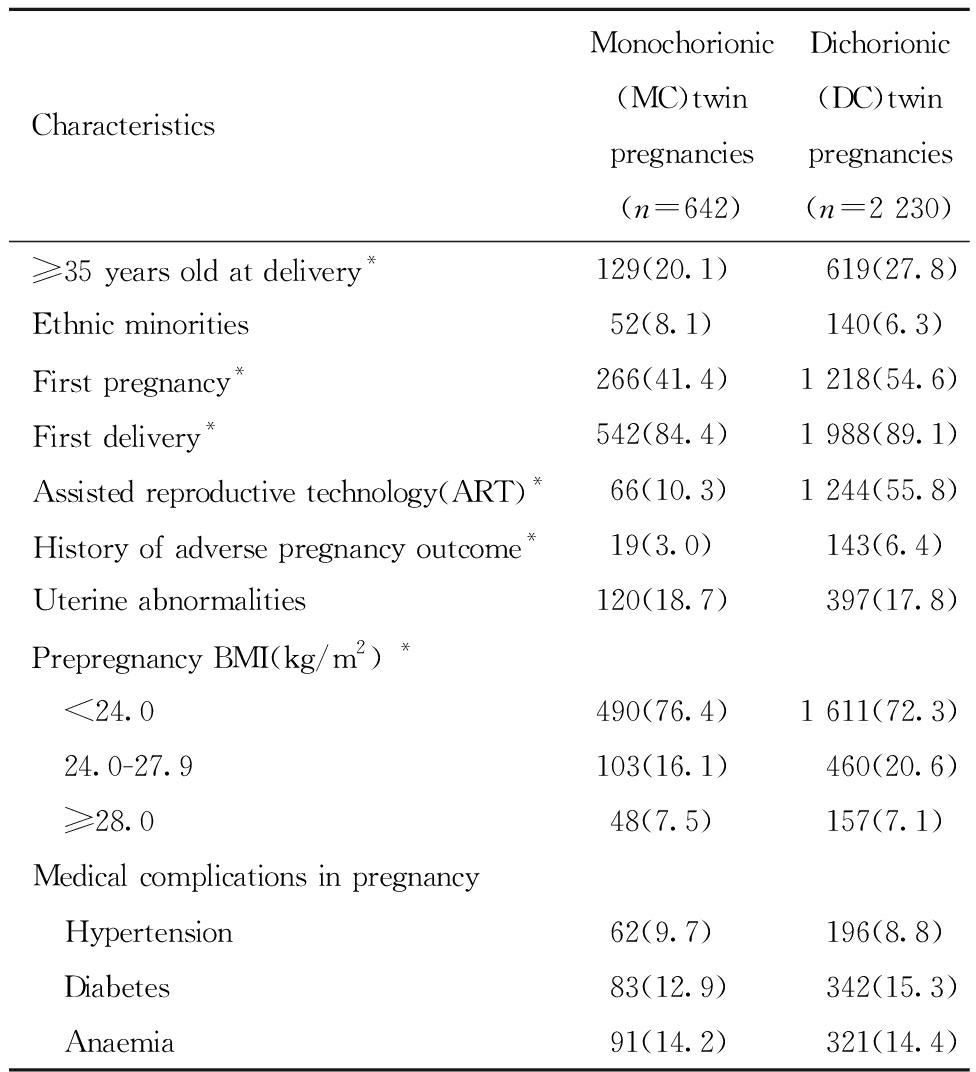
CharacteristicsMonochorionic(MC)twin pregnancies(n=642)Dichorionic(DC)twin pregnancies(n=2 230)≥35 years old at delivery*129(20.1)619(27.8)Ethnic minorities52(8.1)140(6.3)First pregnancy*266(41.4)1 218(54.6)First delivery*542(84.4)1 988(89.1)Assisted reproductive technology(ART)*66(10.3)1 244(55.8)History of adverse pregnancy outcome*19(3.0)143(6.4)Uterine abnormalities120(18.7)397(17.8)Prepregnancy BMI(kg/m2) * <24.0490(76.4)1 611(72.3) 24.0-27.9103(16.1)460(20.6) ≥28.048(7.5)157(7.1)Medical complications in pregnancy Hypertension62(9.7)196(8.8) Diabetes83(12.9)342(15.3) Anaemia91(14.2)321(14.4)
Note:Two-Group Comparison,*P<0.05
二、不同绒毛膜性双胎的子代结局
单绒双胎子代在<28周流产(15.0% vs. 9.0%)和围产期死亡(1.0% vs. 0.4%)、双胎均死亡(包括<28周流产和围产期死亡,12.0% vs. 4.6%)的风险均高于双绒双胎(P均<0.01),早期新生儿死亡(0.2% vs. 0.1%)、出生缺陷(7.3% vs. 6.7%)的发生风险高于双绒双胎但差异无统计学意义(P >0.05),结果见表2。单绒双胎子代不同孕周死亡风险由高到低依次为孕14~27周、孕14周前、孕28~33周和孕34周后,单绒组子代死亡风险均高于双绒组,结果见表3。
表2 不同绒毛膜性双胎妊娠的子代结局 [例(%)]
Table 2 Outcomes of twins with different chorionicity [n(%)]
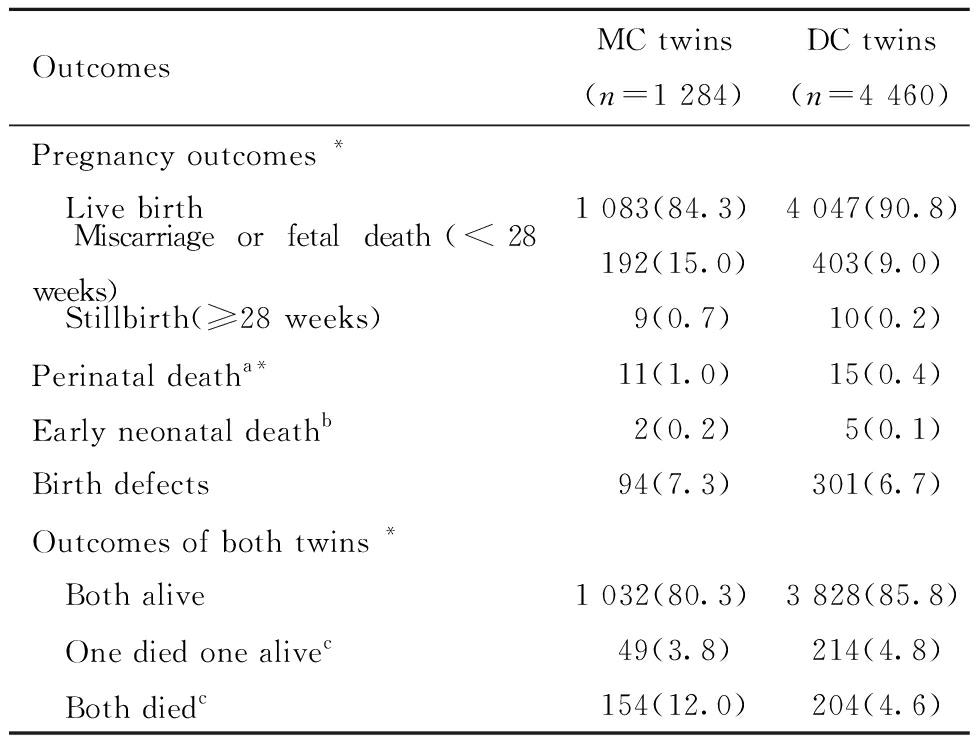
OutcomesMC twins(n=1 284)DC twins(n=4 460)Pregnancy outcomes * Live birth1 083(84.3)4 047(90.8) Miscarriage or fetal death(<28 weeks) 192(15.0) 403(9.0) Stillbirth(≥28 weeks) 9(0.7) 10(0.2)Perinatal deatha* 11(1.0) 15(0.4)Early neonatal deathb 2(0.2) 5(0.1)Birth defects 94(7.3) 301(6.7)Outcomes of both twins * Both alive1 032(80.3)3 828(85.8) One died one alivec 49(3.8) 214(4.8) Both diedc 154(12.0) 204(4.6)
Note:Two-Group Comparison,*P<0.05; a The denominator is the total number of births; b The denominator is the number of live births, and continuous corrected chi-square test is used for difference testing; c Death= miscarriage or fetal death(<28 weeks)+ stillbirth(≥28 weeks)+early neonatal death
表3 不同绒毛膜双胎子代不同孕周死亡风险 [例(%)]
Table 3 Risk of death at different gestational ages for twins with different chorionicity [n(%)]
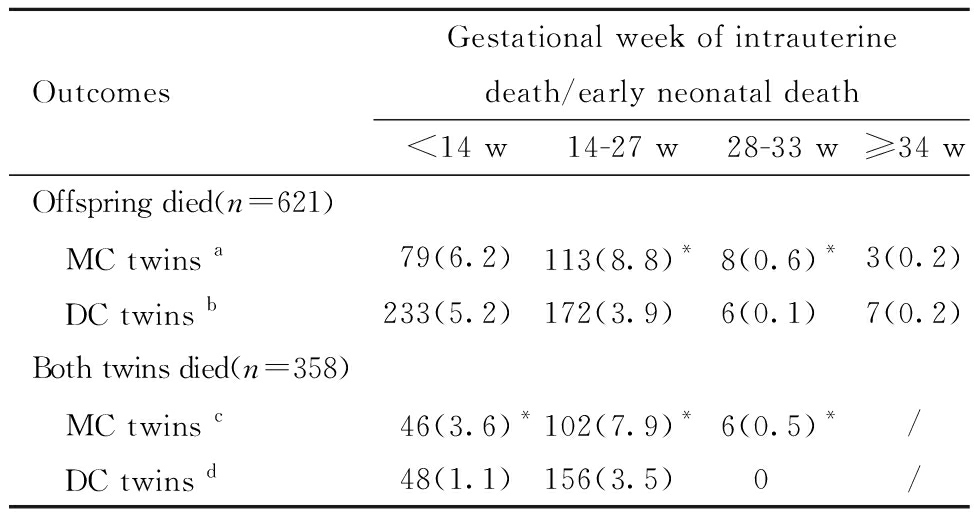
OutcomesGestational week of intrauterine death/early neonatal death<14 w14-27 w28-33 w≥34 wOffspring died(n=621) MC twins a79(6.2)113(8.8)*8(0.6)*3(0.2) DC twins b233(5.2)172(3.9)6(0.1)7(0.2)Both twins died(n=358) MC twins c46(3.6)*102(7.9)*6(0.5)*/ DC twins d48(1.1)156(3.5)0/
Note:Comparison with DC group,*P<0.05; a The denominator is 1 284; therapeutic fetal reduction(21 cases):1 case was <14w , and 20 cases were at 14-27w due to birth defects or complications of MC twins; b The denominator is 4 460; therapeutic fetal reduction(27 cases):10 cases were <14w, 16 cases were at 14~27w and 1 case was at 32w due to birth defect; c The denominator is 1 284; therapeutic fetal reduction(11 cases):11 cases were at 14~27w due to birth defect or complications of MC twins ; d The denominator is 4 460; therapeutic fetal reduction(5 cases):5 cases were at 14-27w due to birth defect.
三、影响不同绒毛膜性双胎子代不良结局危险因素的多因素分析
根据单绒组和双绒组孕母临床特征资料分析中差异有统计学意义因素,结合已有研究结果与临床经验,分别将子代<28周流产、围产期死亡、双胎均死亡和出生缺陷的发生作为结局变量,将是否为单绒双胎妊娠、母亲≥35岁、辅助生殖受孕、孕前BMI≥24.0、既往妊娠史、既往分娩史、既往不良孕产史、子宫异常、孕期合并/并发高血压和糖尿病作为自变量分别纳入二元Logistic回归方程,结果详见表4~表7。结果显示单绒双胎妊娠较双绒双胎妊娠,子代<28周流产、围产期死亡、双胎均死亡风险均增加,比值比(OR)分别为1.85(95%CI:1.50~2.27)、3.22(95% CI:1.45~7.12)和2.71(95% CI:1.91~3.83);子代出生缺陷发生风险差异无统计学意义(OR=1.04,95% CI:0.80~1.35)。此外,孕母≥35岁是发生<28周流产(OR=1.34,95% CI:1.10~1.61)和围产期死亡(OR=2.52,95% CI:1.14~5.55)的独立危险因素,孕前BMI≥24.0是发生<28周流产(OR=1.49,95% CI:1.24~1.78)的独立危险因素,既往有分娩史是发生<28周流产(OR=0.28,95% CI:0.19~0.43)的独立保护因素。
表4 小于28周流产影响因素的多因素非条件Logistic回归分析
Table 4 Multivariate unconditional logistic regression analysis of risk factors of miscarriage or fetal death(<28 weeks)
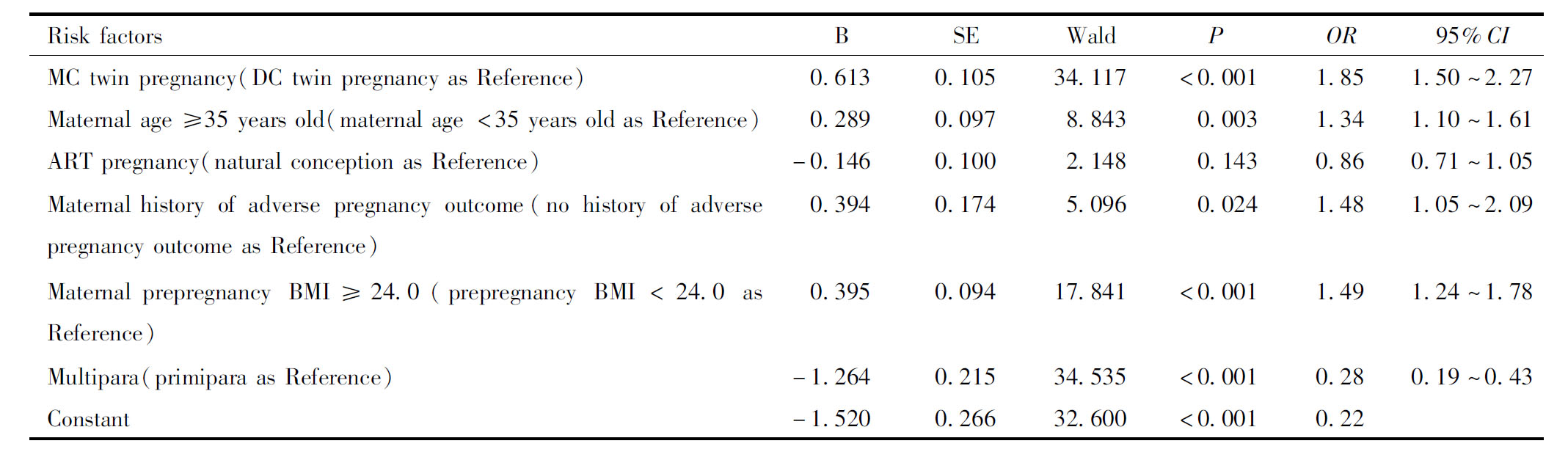
Risk factorsBSEWaldPOR95%CIMC twin pregnancy(DC twin pregnancy as Reference)0.6130.10534.117 <0.0011.851.50~2.27Maternal age ≥35 years old(maternal age <35 years old as Refer-ence)0.2890.0978.8430.0031.341.10~1.61ART pregnancy(natural conception as Reference)-0.1460.1002.1480.1430.860.71~1.05Maternal history of adverse pregnancy outcome(no history of ad-verse pregnancy outcome as Reference)0.3940.1745.0960.0241.481.05~2.09Maternal prepregnancy BMI≥24.0(prepregnancy BMI<24.0 as Reference)0.3950.09417.841<0.0011.491.24~1.78Multipara(primipara as Reference)-1.2640.21534.535<0.0010.280.19~0.43Constant-1.5200.26632.600<0.0010.22
表5 围产期死亡影响因素的多因素非条件Logistic回归分析
Table 5 Multivariate unconditional logistic regression analysis of risk factors of perinatal death

Risk factorsBSEWaldPOR95%CIMC twin pregnancy(DC twin pregnancy as Reference)1.1680.4058.3130.0043.221.45~7.12Maternal age ≥35 years old(maternal age <35 years old as Refer-ence)0.9230.4045.2360.0222.521.14~5.55Multipara(primipara as Reference)-0.6850.742 0.8510.3560.500.12~2.16Maternal history of adverse pregnancy outcome(no history of ad-verse pregnancy outcome as Reference)0.9480.6232.3140.1282.580.76~8.76Maternal hypertension in pregnancy(no hypertension in pregnancy as Reference)0.2380.6190.1480.7001.270.38~4.27Maternal diabetes in pregnancy(no diabetes in pregnancy as Refer-ence)-0.9590.7421.6700.1960.380.09~1.64Constant-5.2020.84537.939<0.0010.01
表6 双胎均死亡影响因素的多因素非条件Logistic回归分析
Table 6 Multivariate unconditional logistic regression analysis of risk factors of death of both twins
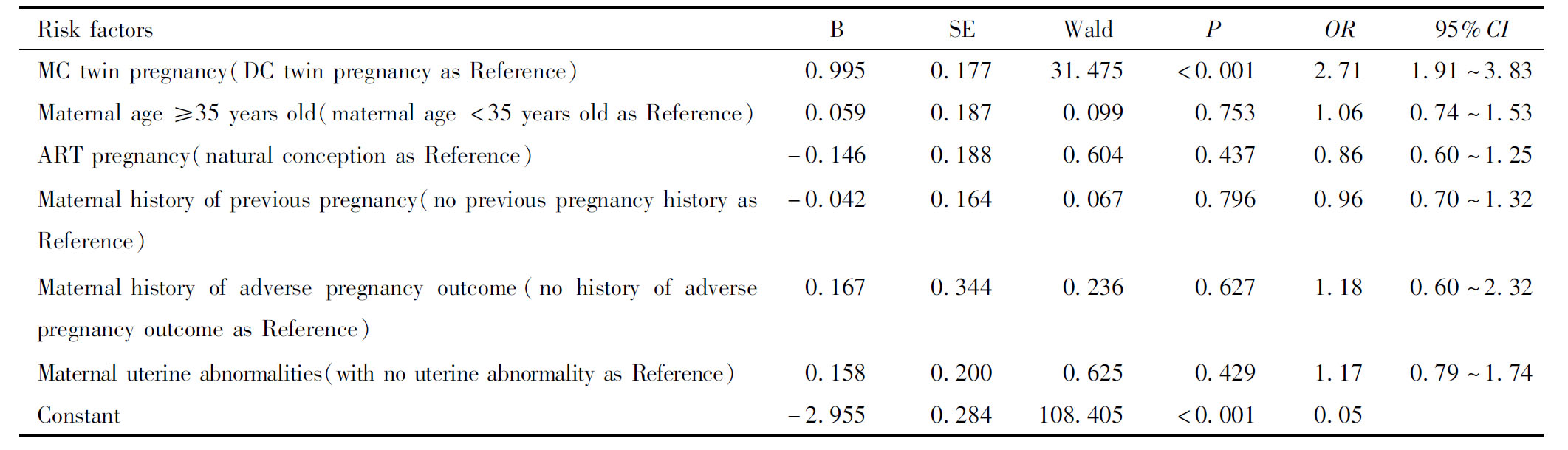
Risk factorsBSEWaldPOR95%CIMC twin pregnancy(DC twin pregnancy as Reference)0.9950.17731.475<0.0012.711.91~3.83Maternal age ≥35 years old(maternal age <35 years old as Refer-ence)0.0590.1870.0990.7531.060.74~1.53ART pregnancy(natural conception as Reference)-0.1460.1880.6040.4370.860.60~1.25Maternal history of previous pregnancy(no previous pregnancy his-tory as Reference)-0.0420.1640.0670.7960.960.70~1.32Maternal history of adverse pregnancy outcome(no history of ad-verse pregnancy outcome as Reference)0.1670.3440.2360.6271.180.60~2.32Maternal uterine abnormalities(with no uterine abnormality as Reference)0.158 0.2000.6250.4291.170.79~1.74Constant-2.9550.284108.405<0.0010.05
表7 出生缺陷影响因素的多因素非条件Logistic回归分析
Table 7 Multivariate unconditional logistic regression analysis of risk factors of birth defects
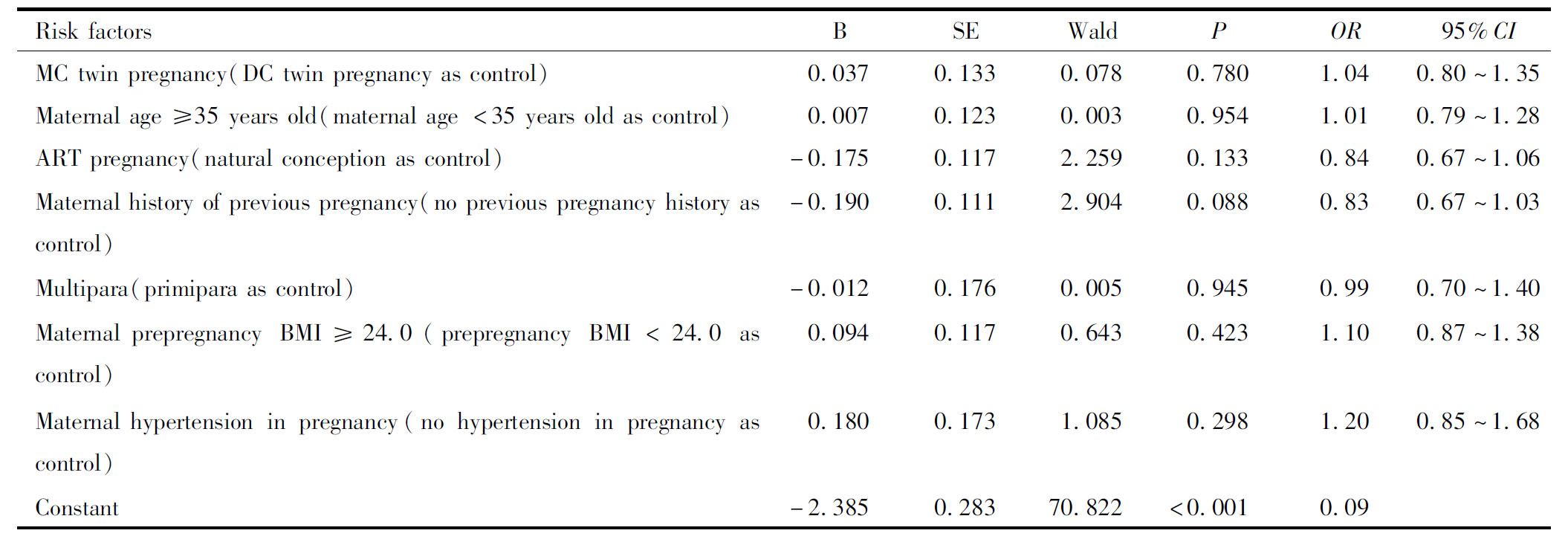
Risk factorsBSEWaldPOR95%CIMC twin pregnancy(DC twin pregnancy as control)0.0370.1330.0780.7801.040.80~1.35Maternal age ≥35 years old(maternal age <35 years old as con-trol)0.0070.1230.0030.9541.010.79~1.28ART pregnancy(natural conception as control)-0.175 0.1172.2590.1330.840.67~1.06Maternal history of previous pregnancy(no previous pregnancy his-tory as control)-0.1900.1112.9040.0880.830.67~1.03Multipara(primipara as control)-0.0120.1760.0050.9450.990.70~1.40Maternal prepregnancy BMI≥24.0(prepregnancy BMI<24.0 as control)0.0940.1170.6430.4231.100.87~1.38Maternal hypertension in pregnancy(no hypertension in pregnancy as control)0.1800.1731.0850.2981.200.85~1.68Constant-2.3850.28370.822<0.0010.09
讨 论
既往研究可知,双绒双胎来自双卵双胎(占全部双胎约70%)和单卵双胎(9%),单绒双胎仅来自单卵双胎(21%)[8]。近年来辅助生殖技术刺激生育力的措施使得双卵双胎(双绒双胎)的发生不断增加[9-11],双绒双胎孕妇中高龄、肥胖、不孕比例较高的特征与使用辅助生殖技术人群的特征基本相符[12-13],而单绒双胎(单卵双胎)更多地出现在自然受孕中[1, 14]。
单绒双胎由于共用胎盘循环,容易发生双胎输血综合征、贫血多血质序列征、动脉反向灌注序列征和选择性胎儿生长受限等并发症,单绒毛膜单羊膜囊双胎因脐带缠绕和打结发生宫内意外的风险更大[14-18]。双胎输血综合征通常在中期妊娠或妊娠16周后逐渐起病,但也可以在之后的妊娠阶段突然起病;贫血多血质序列征和选择性胎儿生长受限则通常在中期妊娠晚期或晚期妊娠起病[19-20]。国内研究显示,单绒毛膜性是发生围产期双胎之一死亡的独立危险因素(OR=2.82,95%CI:1.41~5.64)[21]。国外研究显示在孕11~13周、孕24周后超声显示仍为双活胎的妊娠中,单绒双胎发生至少一胎死亡风险均高于双绒双胎,且一胎死亡后可引起另一胎出现并发症或死亡[8, 22-23],单绒双胎产前至少一个胎儿死亡的风险较双绒双胎高2倍以上。单绒双胎中一胎发生胎死宫内的孕周是影响存活胎儿预后的关键因素,与孕28周后死亡者相比,孕28周前发生一胎死亡者,存活胎儿胎死宫内(OR=2.31,95% CI:1.02~5.25)和新生儿死亡(OR=2.84,95% CI:1.18~6.77)的风险均显著增高[23]。本研究中单绒双胎发生至少一胎死亡的风险明显高于双绒双胎,<28周流产的风险是双绒双胎的1.85倍,28周后围产期死亡的风险是3.22倍;相比于孕早期和孕晚期,孕14~33周单绒双胎发生至少一胎死亡的风险较双绒双胎更高;单绒双胎在整个妊娠期发生子代均死亡的风险也明显高于双绒双胎(2.71倍)。双胎子代不同孕周死亡风险(包括一胎死亡和双胎均死亡)由高到低依次为孕14~27周、孕14周前、孕28~33周和孕34周后,孕28周后发生一胎宫内死亡后另一胎存活几率较孕28周前大。
尽管国外有研究指出单绒双胎妊娠较双绒双胎妊娠早孕期妊娠丢失率升高[24],但由于各国对妊娠妇女开展影像学检查时间的早晚不同或超声筛查水平对绒毛膜性判断的限制,对不同绒毛膜双胎子代孕14周前流产的发生情况缺乏良好的统计数据。本研究中,单绒双胎妊娠孕14周前妊娠丢失率高于双绒双胎妊娠,其中双胎均丢失率更高,且有统计学差异。
此外,既往研究显示单绒双胎较双绒双胎出生缺陷率更高,可能与单绒(单卵)双胎受精卵分裂异常或共用胎盘血管吻合异常而导致畸形有关[25]。单绒双胎先天异常发生率为6.3%,双绒双胎为3.4%。本研究中,单绒双胎出生缺陷率高于双绒双胎(7.3% vs. 6.7%,OR=1.04,95% CI:0.80~1.35),差异无统计学意义,考虑可能与单绒双胎早期流产(<14w)发生率高于双绒双胎有关(6.2% vs.5.2%),一些早期的先天异常尚未被发现。
综上,双胎绒毛膜性对子代不良结局的发生影响较大,单绒双胎妊娠的子代流产、围产期死亡、双胎均死亡和出生缺陷的发生风险均高于双绒双胎妊娠。从中孕期开始,即使在得到更多关注的情况下,单绒双胎出现并发症、出生缺陷和宫内死胎(或治疗性减胎)的风险依然高于双绒双胎,并且在各个孕周发生双胎均死亡的风险也更高。因此,早孕期开始超声筛查并确定绒毛膜性、中孕期加强定期检查和胎儿畸形筛查、晚孕期持续加强对每一个胎儿的关注并适时终止妊娠,对于改善双胎妊娠子代结局,尤其是单绒双胎妊娠,更有积极意义。
1 Stephen T Chasen.Twin pregnancy:Overview.[2022-04-12].http://www.uptodate.com/contents/twin-pregnancy-overview.
2 George T Mandy.Neonatal complications,outcome,and management of multiple births.[2022-04-28].http://www.uptodate.com/contents/neonatal-complications-outcome-and-management-of-multiple-births?
3 Cheong-See F,Schuit E,Arroyo-Manzano D,et al.Prospective risk of stillbirth and neonatal complications in twin pregnancies:systematic review and meta-analysis.BMJ,2016,354:i4353.
4 陆澄秋,肖玲玲,钱蓓倩,等.双胎妊娠新生儿窒息的高危因素.中华围产医学杂志,2021,24:194-199.
5 袁文静,刘惠娜,于俊杰,等.不同绒毛膜性双胎妊娠结局分析.中国实用医刊,2021,48:8-11.
6 张春妤,魏瑗,赵扬玉.单绒毛膜单羊膜囊双胎妊娠的临床特点及妊娠结局分析.中华妇产科杂志,2020,55:627-632.
7 Yu F,Mak A,Chan NM,et al.Prospective risk of stillbirth and neonatal complications for monochorionic diamniotic and dichorionic diamniotic twins after 24 weeks of gestation.J Obstet Gynaecol Res,2021,47:3127-3135.
8 谢幸,孔北华,段涛。妇产科学,第9版.北京:人民卫生出版社,2018:141-146.
9 Martin JA,Hamilton BE,Osterman M,et al.Births:Final Data for 2019.Natl Vital Stat Rep,2021,70:1-51.
10 Zhang L,Zhang W,Xu H,et al.Birth defects surveillance after assisted reproductive technology in Beijing:a whole of population-based cohort study.BMJ Open,2021,11:e044385.
11 杨静薇,邓成艳,黄学锋,等.中华医学会生殖医学分会2018年度辅助生殖技术数据报告.生殖医学杂志,2021,30:419-425.
12 Practice Committee of the American Society for Reproductive Medicine and the Practice Committee for the Society for Assisted Reproductive Technologies.Guidance on the limits to the number of embryos to transfer:a committee opinion.Fertil Steril.2021,116:651-654.
13 孙贻娟,黄国宁,孙海翔,等.关于胚胎移植数目的中国专家共识.生殖医学杂志,2018,27:940-945.
14 王燕芸,王谢桐.含单绒毛膜多胎妊娠的产前管理.中华围产医学杂志,2021,24:245-248.
15 潘育林,崔其亮.双胎发育不均衡的危险因素及妊娠结局.发育医学电子杂志,2020,8:151-156.
16 王佳倞,耿力.单绒毛膜双羊膜囊双胎选择性胎儿生长受限的临床分析.实用妇产科杂志,2020,36:289-293.
17 中华医学会围产医学分会胎儿医学学组,中华医学会妇产科学分会产科学组.双胎妊娠临床处理指南(2020年更新).中华围产医学杂志,2020,23:505-516.
18 Qiao P,Zhao Y,Jiang X,et al.Impact of growth discordance in twins on preeclampsia based on chorionicity.Am J Obstet Gynecol,2020,223:572.e1-572.e8.
19 Jena Miller,Mara Rosner,Ahmet Alexander Baschat.Selective fetal growth restriction in monochorionic twin pregnancies.[2022-02-15].http://www.uptodate.com/contents/selective-fetal-growth-restriction-in-monochorionic-twin-pregnancies?
20 Ramesha Papanna,Eric Bergh.Twin-twin transfusion syndrome_ Screening,prevalence,pathophysiology,and diagnosis.[2022-02-10].http://www.uptodate.com/contents/twin-twin-transfusion-syndrome-screening-prevalence-pathophysiology-and-diagnosis.
21 原婷,王艳艳,田雪叶,等.不同绒毛膜性双胎围产结局717例临床分析.实用妇产科杂志,2020,36:390-394.
22 Litwinska E,Syngelaki A,Cimpoca B,et al.Outcome of twin pregnancy with two live fetuses at 11-13 weeks′ gestation.Ultrasound Obstet Gynecol,2020,55:32-38.
23 Mackie FL,Rigby A,Morris RK,et al.Prognosis of the co-twin following spontaneous single intrauterine fetal death in twin pregnancies:a systematic review and meta-analysis.BJOG,2019,126:569-578.
24 赵建林,石海君,漆洪波.美国妇产科医师学会《多胎妊娠指南(2021版)》要点解读.中国实用妇科与产科杂志,2021,37:1027-1031.
25 George T Mandy.Neonatal complications,outcome,and management of multiple births.[2022-02-14].http://www.uptodate.com/contents/neonatal-complications-outcome-and-management-of-multiple-births?