子痫前期是一种发生于妊娠20周后的复杂疾病综合征,其临床特征是高血压、内皮功能障碍和蛋白尿,导致肝脏、血液、肾脏、大脑等多种母体器官出现衰竭[1-2]。子痫前期使产妇在以后的生活中患心血管疾病的几率大大提升,使胎儿生长受到限制,可能出现肾脏和肝脏等器官功能障碍,是孕产妇和幼儿死亡的主要原因之一[3]。稳定母体和胎儿的状态,然后在双方最佳的时机分娩是目前重度子痫前期唯一的治疗方式[4]。因此,找到一种行之有效的方法判断孕妇是否发生子痫前期、评估疾病的严重程度,从而进行及时的医疗干预,对孕产妇和胎儿具有重要意义。组蛋白去乙酰化酶(histone deacetylases,HDACs)通过从核心组蛋白或非组蛋白中去除乙酰基发挥作用,在大脑、心血管、肌肉、骨骼等多种组织中表达,参与细胞增殖、分化、凋亡以及体内平衡,调节多种生理过程[5]。HDACs根据其蛋白质结构、功能和亚细胞定位分为Ⅰ类和Ⅱ类,HDAC4、HDAC6同属于Ⅱ类,具有组织特异性[6]。HDAC4在细胞核和细胞质中都有表达,通过介导多种细胞反应,在神经退行性病变、心血管疾病、肌肉萎缩等多种疾病中发挥重要作用[7]。HDAC6是一种结构和功能独特的细胞质脱乙酰酶,主要定位于细胞质中,在癌症、炎症、神经变性、神经系统疾病中发挥重要的作用[8]。然而,目前HDAC4、HDAC6与子痫前期发生及病情严重程度的关系至今未见报道。因此,本研究通过检测子痫前期患者血清HDAC4、HDAC6表达水平,分析二者与子痫前期发生和病情严重程度的关系,为子痫前期的有效诊治和预后改善提供参考依据。
对象与方法
一、研究对象
选取西北妇女儿童医院2020年1月—2021年6月期间住院治疗的80例子痫前期患者(子痫前期组)。根据患者病情的严重程度[9]分为轻度组(n=48)和重度组(n=32)。纳入标准:(1)符合子痫前期相关诊断标准[10];(2)自然受孕,单胎妊娠;(3)有规律产检和临床资料完整;(4)研究对象本人详知此项研究内容,并自愿签署同意书。排除标准:(1)伴有心脏病或其他心血管疾病的孕妇;(2)伴有肝病、肾病及糖尿病等疾病的孕妇;(3)伴有免疫性疾病、实质器官病变及血液性等基础疾病的孕妇;(4)病例资料不完整患者。本研究经本院伦理委员会批准(批号:2020-009),遵循《世界医学协会赫尔辛基宣言》。另选取同期产检并住院分娩且一般资料与子痫前期组相匹配的健康孕妇80例为对照组。收集子痫前期组和对照组的年龄、体重指数、收缩压、舒张压、产次、孕次、孕周、新生儿体质量等基本资料。
二、方法
1.样本收集:子痫前期患者和对照组孕妇,静脉采血约3~5 mL,离心半径为12 cm,时间为10 min,分离血清后,放入-20 ℃冰箱中保存,待检。收集两组24 h尿液,检测24 h尿蛋白定量。
2.检测血清HDAC4、HDAC6水平:采用Varioskan LUX多功能酶标仪(美国赛默飞公司),于450nm处,用酶联免疫吸附法检测HDAC4、HDAC6水平,HDAC4酶联免疫试剂盒(货号:ml059922)、HDAC6酶联免疫试剂盒(货号:ml028648)均购自上海酶联生物科技有限公司。
3.统计学方法:数据以SPSS 25.0软件进行统计学分析,经正态性检验,符合正态分布,以![]() 描述,采用独立样本t检验进行组间计量资料比较;Pearson法分析子痫前期患者血清HDAC4、HDAC6水平和疾病严重程度之间的相关性以及子痫前期患者血清HDAC4水平与HDAC6水平的相关性;多因素Logistic回归分析影响孕妇发生子痫前期的因素;ROC曲线分析血清HDAC4、HDAC6水平预测孕妇发生子痫前期的价值,P<0.05表示差异有统计学意义。
描述,采用独立样本t检验进行组间计量资料比较;Pearson法分析子痫前期患者血清HDAC4、HDAC6水平和疾病严重程度之间的相关性以及子痫前期患者血清HDAC4水平与HDAC6水平的相关性;多因素Logistic回归分析影响孕妇发生子痫前期的因素;ROC曲线分析血清HDAC4、HDAC6水平预测孕妇发生子痫前期的价值,P<0.05表示差异有统计学意义。
结 果
一、两组一般临床资料比较
与对照组相比,子痫前期患者收缩压、舒张压、24 h尿蛋白定量、总胆固醇、甘油三脂、HDAC4、HDAC6显著升高(P<0.05),年龄、体重指数、产次、孕次、孕周、新生儿体质量均无显著性差异(P>0.05)。见表1。
表1 两组一般临床资料比较
Table 1 Comparison of general clinical data between the two groups
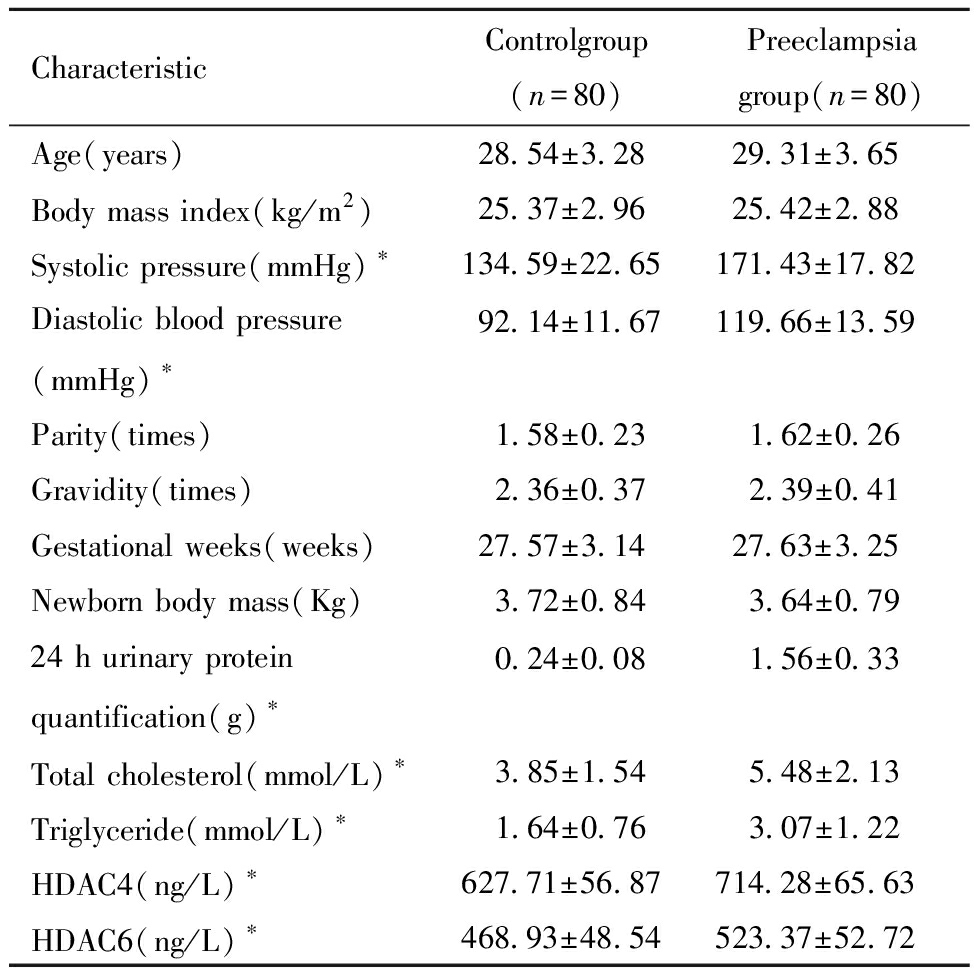
CharacteristicControlgroup(n=80)Preeclampsia group(n=80)Age(years)28.54±3.2829.31±3.65Body mass index(kg/m2)25.37±2.9625.42±2.88Systolic pressure(mmHg)∗134.59±22.65171.43±17.82Diastolic blood pressure(mmHg)∗92.14±11.67119.66±13.59Parity(times) 1.58±0.23 1.62±0.26Gravidity(times) 2.36±0.37 2.39±0.41Gestational weeks(weeks)27.57±3.1427.63±3.25Newborn body mass(Kg) 3.72±0.84 3.64±0.7924 h urinary protein quantification(g)∗ 0.24±0.08 1.56±0.33Total cholesterol(mmol/L)∗ 3.85±1.54 5.48±2.13Triglyceride(mmol/L)∗ 1.64±0.76 3.07±1.22HDAC4(ng/L)∗627.71±56.87714.28±65.63HDAC6(ng/L)∗468.93±48.54523.37±52.72
Comparison between two groups,*P<0.05
二、不同严重程度的子痫前期患者血清HDAC4、HDAC6水平比较
与轻度组相比,重度组HDAC4、HDAC6表达水平显著升高(P<0.05)。见表2。
表2 不同严重程度的子痫前期患者血清HDAC4、HDAC6水平比较
Table 2 Comparison of serum HDAC4 and HDAC6 levels in patients with preeclampsia of different severity
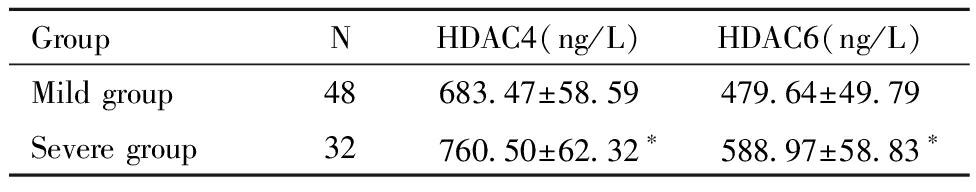
GroupNHDAC4(ng/L)HDAC6(ng/L)Mild group48683.47±58.59479.64±49.79Severe group32760.50±62.32∗588.97±58.83∗
Comparison between two groups,*P<0.05
三、血清HDAC4、HDAC6水平和病情严重程度相关性分析
以血清HDAC4、HDAC6水平和病情严重程度为双变量进行相关性分析,变量赋值:轻度=1,重度=2,结果显示血清HDAC4与病情严重程度呈显著正相关(r=0.536,P=0.000),HDAC6水平与病情严重程度呈显著正相关(r=0.614,P<0.001)。
Pearson法分析显示,子痫前期患者血清HDAC4水平与HDAC6水平呈显著正相关(r=0.412,P<0.001)。见图1。
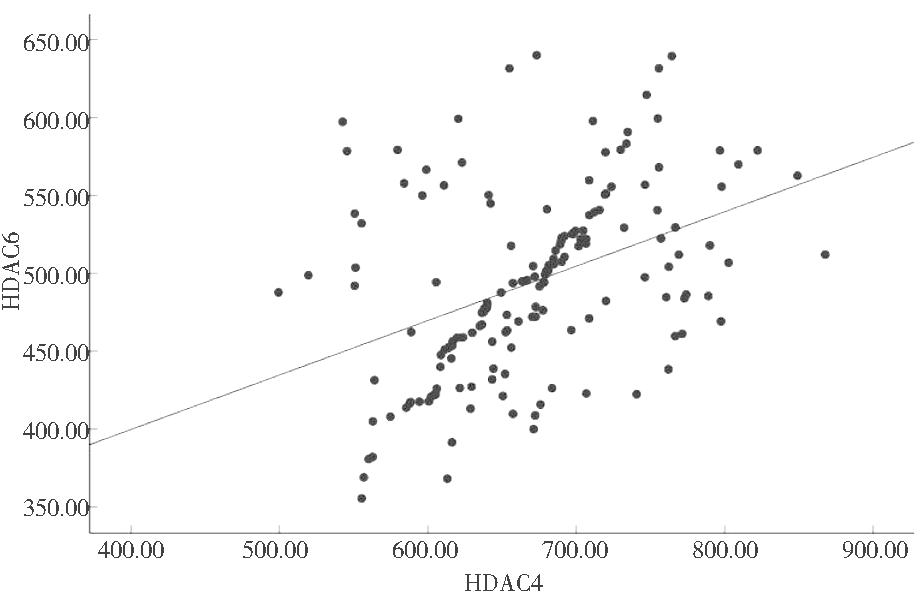
图1 子痫前期患者血清HDAC4水平与HDAC6水平的相关性
Figure 1 Correlation between serum HDAC4 levels and HDAC6 levels in patients with preeclampsia
四、多因素Logistic回归分析孕妇发生子痫前期的影响因素
以孕妇是否发生子痫前期为因变量(是=1,否=0),以血清HDAC4、HDAC6、收缩压、舒张压、24 h尿蛋白定量、总胆固醇、甘油三脂(连续变量)为自变量进行多因素Logistic回归分析,结果显示,血清HDAC4、HDAC6、收缩压、舒张压、24 h尿蛋白定量、总胆固醇、甘油三脂是子痫前期发生的影响因素(P<0.05)。见表3。
表3 多因素Logistic回归分析孕妇发生子痫前期的影响因素
Table 3 Multivariate Logistic regression analysis of influencing factors of preeclampsia in pregnant women
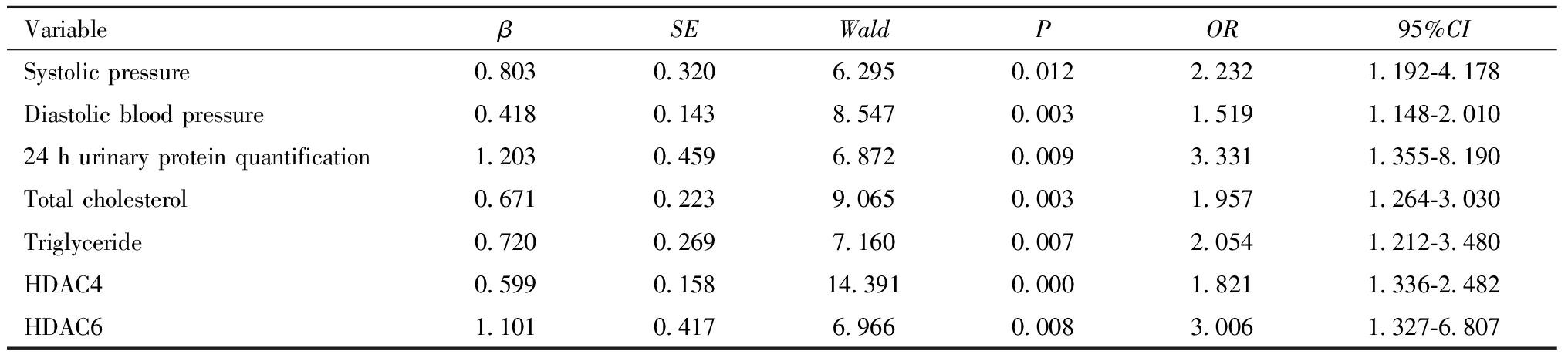
VariableβSEWaldPOR95%CISystolic pressure0.8030.3206.2950.0122.2321.192-4.178Diastolic blood pressure0.4180.1438.5470.0031.5191.148-2.01024 h urinary protein quantification1.2030.4596.8720.0093.3311.355-8.190Total cholesterol0.6710.2239.0650.0031.9571.264-3.030Triglyceride0.7200.2697.1600.0072.0541.212-3.480HDAC40.5990.15814.3910.0001.8211.336-2.482HDAC61.1010.4176.9660.0083.0061.327-6.807
五、血清HDAC4、HDAC6对发生子痫前期的预测价值
HDAC4预测发生子痫前期的曲线下面积(area under curve,AUC)为0.828;血清HDAC6预测发生子痫前期的AUC为0.752;二者联合预测发生子痫前期的AUC为0.886,优于HDAC4、HDAC6各自单独预测(Z联合检测-HDAC4=2.564、Z联合检测-HDAC6=4.083,P均<0.05)。见表4和图2。
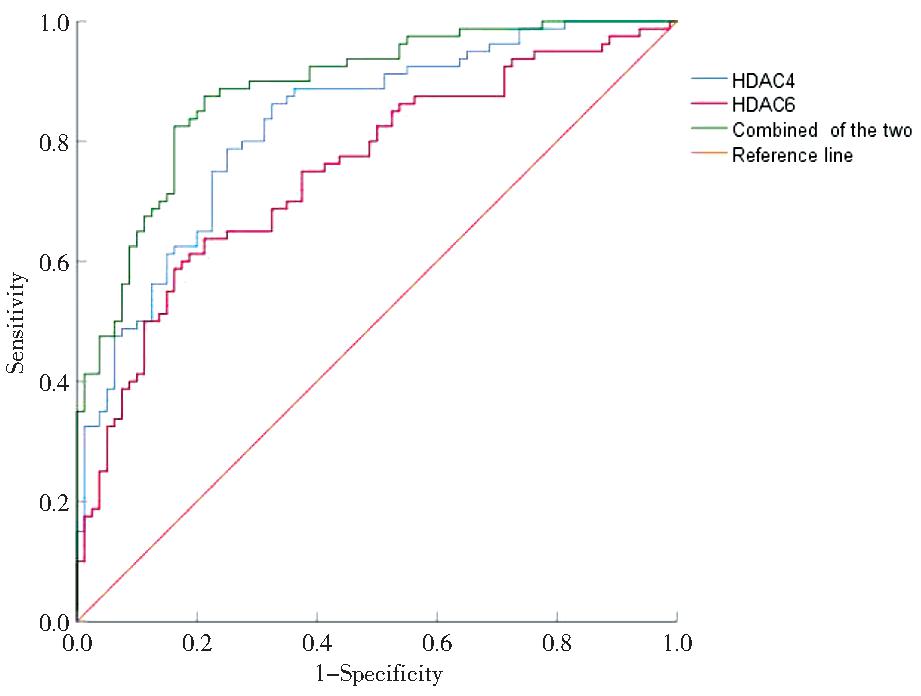
图2 血清HDAC4、HDAC6水平预测子痫前期发生的ROC曲线
Figure 2 ROC curve of serum HDAC4 and HDAC6 levels predicting preeclampsia
表4 血清HDAC4、HDAC6对孕妇发生子痫前期的预测价值
Table 4 The predictive value of serum HDAC4 and HDAC6 in the occurrence of preeclampsia in pregnant women
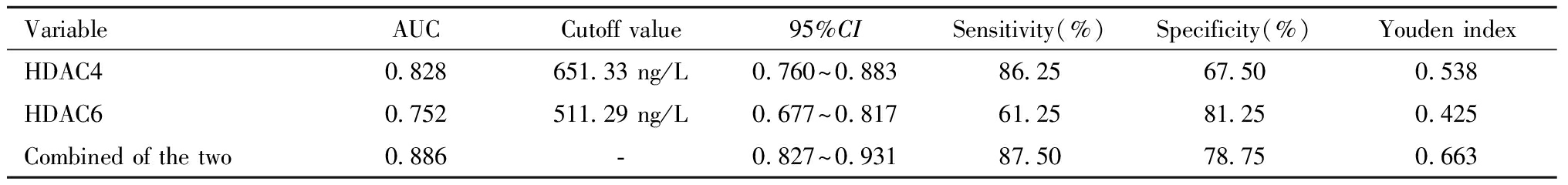
VariableAUCCutoff value95%CISensitivity(%)Specificity(%)Youden indexHDAC40.828651.33 ng/L0.760~0.88386.2567.500.538HDAC60.752511.29 ng/L0.677~0.81761.2581.250.425Combined of the two0.886-0.827~0.93187.5078.750.663
讨 论
子痫前期是一种由胎盘、血管、肾脏、免疫功能障碍等多种因素引起的综合征,不止有一种亚型,各种病理生理途径都会导致母婴死亡率和发病率增加[11]。目前,子痫前期的发病机制尚不清楚,影响全世界约5%~7%的妊娠,如果治疗不及时,可能会导致母体和婴儿出现严重的并发症,造成终生残疾,甚至死亡[12]。因此,迫切需要寻找有效的与临床相关的诊断标志物,准确识别孕妇是否发生子痫前期、评估疾病的严重程度,以便及时调整临床治疗策略、控制病情,这对子痫前期的早发现、早治疗具有重大的现实意义。
HDACs通过基因转录和调节组蛋白修饰,对人类疾病的发展产生广泛影响[13]。HDAC4属于HDAC Ⅱa类,在细胞和组织中的生理和病理过程中起着重要的作用[14]。Cheng等[15]发现HDAC4加速细胞周期G1/S转变,并诱导上皮-间充质转变以促进鼻咽癌细胞增殖、迁移和体外侵袭,以及体内肿瘤生长和肺转移。Dou等[16]发现HDAC4可以调节T辅助细胞17的分化,通过增加促炎细胞因子的表达水平从而造成强直性脊柱炎严重程度的加重,在强直性脊柱炎的发生发展中起着至关重要的作用。本研究结果显示,子痫前期患者血清HDAC4水平显著高于对照组,重度组HDAC4表达水平显著高于轻度组,提示血清HDAC4水平对于初步判断子痫前期的发生和病情严重程度具有一定的意义。
HDAC6属于HDAC Ⅱb类,是唯一具有两个串联催化结构域的HDAC亚型,有一个类似水解酶的锌指结构域,可结合和运输多聚泛素化蛋白聚集体,以及一个可以调节蛋白质-蛋白质互作的结构域受体[17-18]。Zhou等[19]发现HDAC6是食管癌、结直肠癌、胰腺癌等多种胃肠道癌症的致癌基因。Guo等[20]发现HDAC6促进了盲肠结扎穿孔引起的败血症的发展,抑制HDAC6的表达可以通过抑制线粒体功能障碍和减少氧化剂的产生,显著减轻盲肠结扎穿孔引起的败血症,从而保护大鼠免受氧化损伤。本研究结果发现,与对照组相比,子痫前期患者血清HDAC6水平显著升高,重度组HDAC6表达水平显著高于轻度组,相关性分析显示血清HDAC4、HDAC6分别与病情严重程度呈显著正相关(r=0.536、0.614),提示血清HDAC4、HDAC6有望成为子痫前期发生和评估病情严重程度的潜在标志物。Wu等[21]发现HDAC4心力衰竭大鼠的左心室高表达,HDAC6基因表达增加与心脏纤维化密切相关。Kee等[22]发现HDAC4、HDAC6通过调节血管肥大、血管收缩、炎症或氧化应激,与老龄高血压人群中不良反应有关。Pearson相关分析显示,子痫前期患者血清HDAC4水平与HDAC6水平呈显著正相关。ROC曲线显示,HDAC4、HDAC6二者联合预测发生子痫前期的AUC为0.886,优于HDAC4、HDAC6各自单独预测,表明HDAC4、HDAC6可能通过调节血管和心脏纤维化,与心脏功能和高血压密切相关,可以作为孕妇发生子痫前期疾病的生物标志物,二者联合对预测孕妇发生子痫前期具有重要指导价值。
子痫前期是以高血压和蛋白尿为主要临床特征的疾病,孕妇随着孕周增加血脂水平逐渐升高,过高的血脂在胎盘血管内皮沉积可能会导致血管内皮的损伤,24 h尿蛋白定量是临床上常用的诊断子痫前期并评价其病情的指标[21-22]。本研究多因素Logistic回归分析结果显示,血清HDAC4、HDAC6、收缩压、舒张压、24 h尿蛋白定量、总胆固醇、甘油三脂是孕妇发生子痫前期的影响因素,提示应密切关注上述因素,以便及时对患者采取干预措施。
综上所述,血清HDAC4、HDAC6水平可以反映孕妇是否发生子痫前期以及疾病的严重程度,二者联合对评估孕妇是否发生子痫前期有较好参考价值。然而HDAC4、HDAC6参与子痫前期发生发展的具体机制,仍需进一步研究,与患者分娩结局的关系尚需后续随访。
1 Turbeville HR,Sasser JM.Preeclampsia beyond pregnancy:long-term consequences for mother and child.Am J Physiol Renal Physiol,2020,318:1315-1326.
2 MacDonald TM,Walker SP,Hannan NJ,et al.Clinical tools and biomarkers to predict preeclampsia.EBioMedicine,2022,75:1-10.
3 Rana S,Lemoine E,Granger JP,et al.Preeclampsia:pathophysiology,challenges,and perspectives.Circ Res,2019,124:1094-1112.
4 林雪燕,杨孜,史峻梅,等.不同转诊时机对转诊系统内重度子痫前期孕妇妊娠结局的影响.中华妇产科杂志,2022,57:143-171.
5 Ha N,Sun J,Bian Q,et al.Hdac4 regulates the proliferation of neural crest-derived osteoblasts during murine craniofacial development.Front Physiol,2022,13:1-10.
6 Imran M,Shafiq S,Naeem MK,et al.Histone deacetylase (HDAC) gene family in allotetraploid cotton and its diploid progenitors:in silico identification,molecular characterization,and gene expression analysis under multiple abiotic stresses,DNA damage and phytohormone treatments.Int J Mol Sci,2020,21:1-19.
7 Huang C,Lin Z,Liu X,et al.HDAC4 inhibitors as antivascular senescence therapeutics.Oxid Med Cell Longev,2022,3:1-12.
8 Iaconelli J,Xuan L,Karmacharya R.HDAC6 modulates signaling pathways relevant to synaptic biology and neuronal differentiation in human stem-cell-derived neurons.Int J Mol Sci,2019,20:1-18.
9 蔡雁,王晓莹.如何监测、预防子痫前期走向重度.中国实用妇科与产科杂志,2018,34:520-525.
10 中华医学会妇产科学分会妊娠期高血压疾病学组.妊娠期高血压疾病诊治指南(2020).中华妇产科杂志,2020,55:227-238.
11 Roberts JM,Rich-Edwards JW,McElrath TF,et al.Subtypes of preeclampsia:recognition and determining clinical usefulness.Hypertension,2021,77:1430-1441.
12 Jena MK,Sharma NR,Petitt M,et al.Pathogenesis of preeclampsia and therapeutic approaches targeting the placenta.Biomolecules,2020,10:1-25.
13 Gong M,Yu Y,Liang L,et al.HDAC4 mutations cause diabetes and induce β-cell FoxO1 nuclear exclusion.Mol Genet Genomic Med,2019,7:1-10.
14 Shen F,Hou X,Li T,et al.Pharmacological and genetic inhibition of HDAC4 alleviates renal injury and fibrosis in mice.Front Pharmacol,2022,13:1-15.
15 Cheng C,Yang J,Li SW,et al.HDAC4 promotes nasopharyngeal carcinoma progression and serves as a therapeutic target.Cell Death Dis,2021,12:1-15.
16 Dou B,Ma F,Jiang Z,et al.Blood HDAC4 variation links with disease activity and response to tumor necrosis factor inhibitor and regulates CD4+ T cell differentiation in ankylosing spondylitis.Front Med (Lausanne),2022,9:1-11.
17 LoPresti P.HDAC6 in Diseases of Cognition and of Neurons.Cells,2020,10:1-15.
18 Chang P,Li H,Hu H,et al.The Role of HDAC6 in Autophagy and NLRP3 Inflammasome.Front Immunol,2021,12:1-13.
19 Zhou B,Liu D,Tan Y.Role of HDAC6 and its selective inhibitors in gastrointestinal cancer.Front Cell Dev Biol,2021,9:1-10.
20 Guo SD,Yan ST,LiW,et al.HDAC6 promotes sepsis development by impairing PHB1-mediated mitochondrial respiratory chain function.Aging (Albany NY),2020,12:5411-5422.
21 Wu Y,Si F,Luo L,et al.The effect of melatonin on cardio fibrosis in juvenile rats with pressure overload and deregulation of HDACs.Korean J Physiol Pharmacol,2018,22:607-616.
22 Kee HJ,Kim I,Jeong MH.Zinc-dependent histone deacetylases:Potential therapeutic targets for arterial hypertension.Biochem Pharmacol,2022,202:1-15.
23 瞿琳,周欣,殷茵,等.子痫前期患者24 h尿蛋白定量与其不良妊娠结局的相关性临床研究.南京医科大学学报(自然科学版),2022,42:216-221.
24 韩雪杰,张松,李悦.子痫前期与心血管病关系的研究进展.中华高血压杂志,2019,27:421-425.